Chronic non-healing wounds such as diabetic foot ulcers and venous insufficiency ulcers remain in the inflammatory state despite adequate management, prolonging wound healing, and adversely affecting the quality of life of patients. While pathologies vary, one of the most frequent causes is hypoxic (low-oxygenated) wound tissues in the wound bed. Hyperbaric oxygen wound therapy (HBOT) has gained attention as a viable procedure for treating select wounds in the medical community for many years. This article will examine the procedure, benefits, limitations, and contraindications of HBOT in managing chronic wounds.
What is HBOT?
Hyperbaric oxygen wound therapy is a wound management technique where a patient's body is exposed to 100% oxygen at a pressure higher than atmospheric pressure for a short period. It improves oxygenation in chronic wounds where other methods fail, thus increasing the rate of wound healing. Adequate and timely treatment of chronic wounds using HBOT may also help to prevent the need for partial or total lower limb amputation.
Procedure
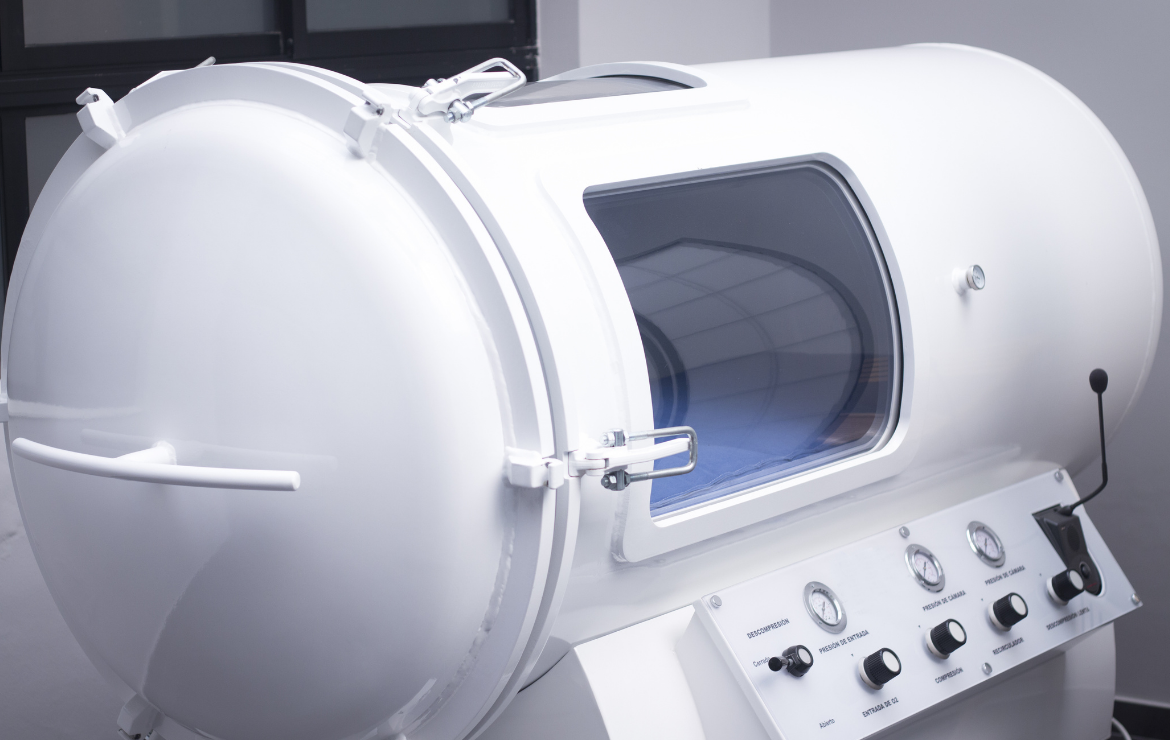
Hyperbaric oxygen wound therapy is administered inside a chamber subjected to significantly higher pressures than atmospheric pressure. According to Henry’s law, the quantity of oxygen from the immediate environment that dissolves in the blood or body tissue is proportional to the partial pressure. Thus, hyperbaric conditions can increase the amount of oxygen available in skin tissues, which is critical for wound healing.
Hyperbaric chambers are typically monoplace or multi-place tubes up to 7 feet long fitted with a hood or mask that allows a patient to breathe 100% oxygen intermittently while the rest of the body (including wounds) is exposed. The chamber is subsequently pressurized to 2.5 or 3 times the atmospheric pressure between 30 minutes and 2 hours and slowly depressurized. Depending on the nature and severity of the wound, the treatment may be administered more than once a day.
The primary mechanisms of action in HBOT are hyperoxygenation and reduction of bubble size. An increase in the amount of dissolved oxygen in the wound bed results in a corresponding increase in collagen synthesis and fibroblast proliferation. A reduction in the bubble size due to increased pressure in the hyperbaric chamber aids the management of decompression sickness in patients. Secondary mechanisms include angiogenesis, inhibition of toxins, vasoconstriction, and increasing free radical formation.
Benefits of HBOT
HBOT has been established as a viable technique for treating chronic wounds where other methods fail. HBOT can be administered to manage the following wound types:
Diabetic foot ulcers, venous insufficiency ulcers, and other ischemic wounds
When used in treating chronic wounds such as diabetic foot ulcers and venous ulcers, HBOT increases the rate of wound healing by improving angiogenesis and stimulating growth factors, notably the vascular endothelial growth factor (VEGF). HBOT is usually administered alongside other wound management techniques such as dressings, pressure relief, infection control, debridement, and nutrition.
Compromised skin grafts and flaps
In compromised skin grafts and flaps, HBOT facilitates wound healing by inducing hyperoxia in the wound bed as well as enhancing leukocyte function, angiogenesis, and antimicrobial action. Further, HBOT improves oxygenation in the grafts to improve survival and induces fibroblast proliferation and collagen synthesis in compromised flaps.
Necrotizing soft tissue infections and radiation-induced wounds
For treating infected wounds such as necrotizing soft tissues and clostridial myonecrosis, HBOT induces antimicrobial action by inhibiting the production of toxins through the production of oxidative free radicals. HBOT will be typically administered alongside surgical debridement and antibiotics for infection control. In radiation-induced wounds, HBOT improves oxygenation in the irradiated tissues and also acts as a catalytic factor for angiogenesis.
Contraindications of HBOT
Despite numerous benefits for promoting wound healing in chronic wounds, HBOT has several side effects and may result in complications in patients. Common side effects and complications post-therapy include myopia, lung damage, rupture of the middle ear, decompression sickness, seizures, aggravation of existing cataracts, and hypoglycemia. Barotrauma (pressure-induced injuries), in particular, result from the body’s inability to equalize pressure from the chamber with the surrounding environment for a period after the procedure. Tissue related injury occurs due to excessive shear force induced by the expansion of gas within the chamber, or pressure hydrostatic pressure transmission through tissue. In most cases, however, HBOT side effects will resolve on their own anywhere from a few days to weeks.


.webp)

.avif)