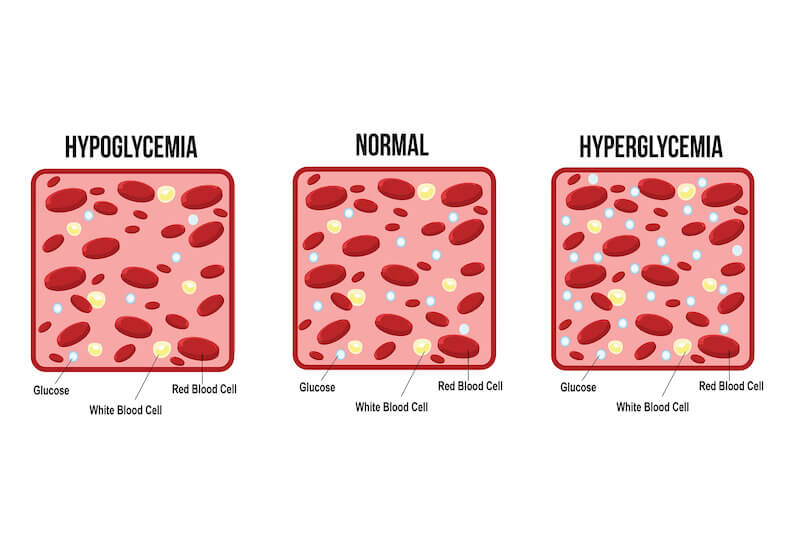
Hypoglycemia and hyperglycemia are two distinct conditions characterized by abnormal blood sugar levels. Hypoglycemia occurs when blood sugar levels drop below normal, typically defined as below 70 milligrams per deciliter (mg/dL). On the other hand, hyperglycemia occurs when blood sugar levels are higher than usual, often exceeding 180 mg/dL. While both conditions involve fluctuations in blood sugar, they have different causes, symptoms, and treatment approaches.
Importance of Distinguishing Between the Two
Distinguishing between hypoglycemia and hyperglycemia is crucial for proper management and treatment. Misidentifying the condition can lead to inappropriate interventions and potential complications. Hypoglycemia requires immediate action to raise blood sugar levels to prevent serious consequences such as loss of consciousness or seizures. Conversely, hyperglycemia necessitates adjustments in medication, diet, and lifestyle to lower blood sugar levels and reduce the risk of long-term complications associated with diabetes. Understanding the differences between hypoglycemia and hyperglycemia enables individuals to recognize symptoms, take appropriate action, and maintain optimal blood sugar control for overall health and well-being.
What is Hypoglycemia?
Definition and Characteristics
Hypoglycemia, often called low blood sugar, occurs when the glucose levels in the blood drop below normal levels, typically below 70 milligrams per deciliter (mg/dL). Glucose is the primary energy source for the body's cells, including the brain, so maintaining stable blood sugar levels is crucial for overall health and function. When blood sugar levels become too low, the body may not have enough energy to function correctly, leading to various symptoms.
Normal Blood Sugar Levels
Normal blood sugar levels typically range between 70 to 99 mg/dL when fasting and rise to around 140 mg/dL after meals. However, these levels can vary depending on individual factors such as age, health status, and time of day. Maintaining blood sugar within this range ensures the body has a steady energy supply to support various physiological processes.
Causes of Hypoglycemia
Hypoglycemia can be caused by several factors, including excessive insulin production, inadequate food intake, excessive physical activity, and certain medical conditions or medications. In people with diabetes, hypoglycemia often occurs as a result of taking too much insulin or other glucose-lowering medications without consuming enough carbohydrates to balance it. Other causes of hypoglycemia include alcohol consumption, hormone deficiencies, liver or kidney disorders, and certain rare genetic disorders.
Risk Factors and Complications
Several risk factors increase the likelihood of experiencing hypoglycemia, including diabetes, certain medications (such as insulin or sulfonylureas), skipping meals or eating irregularly, excessive alcohol consumption, and strenuous physical activity. Complications of hypoglycemia can range from mild to severe and may include confusion, dizziness, shakiness, sweating, rapid heartbeat, seizures, unconsciousness, and even death if left untreated. Recurrent episodes of hypoglycemia can also lead to impaired awareness of low blood sugar and increase the risk of severe hypoglycemic events. Therefore, individuals at risk of hypoglycemia need to monitor their blood sugar levels regularly, follow a balanced diet, and adjust medication doses as required under the guidance of a healthcare provider.
What is Hyperglycemia?
Definition and Characteristics
Hyperglycemia, also known as high blood sugar, occurs when the glucose levels in the blood rise above normal levels, typically exceeding 180 milligrams per deciliter (mg/dL) in individuals with diabetes. Elevated blood sugar levels can result from insufficient insulin production, impaired insulin function, or a combination of both. Excess sugar accumulates in the bloodstream without adequate insulin to help glucose enter cells for energy, leading to hyperglycemia.
Normal Blood Sugar Levels
Normal blood sugar levels typically range between 70 to 99 mg/dL when fasting and rise to around 140 mg/dL after meals. However, individuals with diabetes may have higher target ranges for blood sugar control, often aiming for levels below 180 mg/dL to minimize the risk of hyperglycemia-related complications. Maintaining blood sugar within target ranges is essential for preventing long-term complications associated with diabetes, such as heart disease, kidney disease, nerve damage, and vision problems.
Causes of Hyperglycemia
Hyperglycemia can occur for various reasons, including inadequate insulin production by the pancreas, insulin resistance (where cells do not respond effectively to insulin), excessive carbohydrate intake, stress, illness or infection, certain medications (such as corticosteroids), and hormonal imbalances. In individuals with diabetes, hyperglycemia often occurs due to factors such as missed insulin doses, insufficient insulin dosage, poor diet choices, lack of physical activity, or changes in medication or treatment regimens. Understanding the underlying causes of hyperglycemia is essential for effectively managing blood sugar levels and reducing the risk of complications.
Risk Factors and Complications
Several risk factors increase the likelihood of developing hyperglycemia, including having diabetes (type 1 or type 2), obesity, a sedentary lifestyle, a family history of diabetes, aging, certain medical conditions (such as polycystic ovary syndrome or thyroid disorders), and stress. Complications of hyperglycemia can be acute or chronic. They may include increased thirst and urination, blurred vision, fatigue, slow wound healing, frequent infections, diabetic ketoacidosis (DKA), hyperosmolar hyperglycemic state (HHS), cardiovascular disease, nerve damage, and kidney damage. Managing blood sugar levels through medication, diet, exercise, and regular monitoring is essential for preventing hyperglycemia-related complications and maintaining overall health and well-being.
What Causes Hypoglycemia And Hyperglycemia?
Underlying Health Conditions
Hypoglycemia:
Hypoglycemia can occur as a result of various underlying health conditions that affect blood sugar regulation. These may include:
a. Diabetes: Individuals with diabetes, particularly those treated with insulin or certain oral medications, are at increased risk of hypoglycemia due to medication-induced drops in blood sugar levels.
b. Insulinoma: Insulinoma is a rare tumor of the pancreas that produces excessive amounts of insulin, leading to hypoglycemia.
c. Liver Disease: Liver diseases such as hepatitis, cirrhosis, or liver failure can impair the liver's ability to store and release glucose, resulting in hypoglycemia.
d. Adrenal Insufficiency: Adrenal insufficiency, a condition characterized by inadequate production of adrenal hormones, can lead to hypoglycemia due to reduced cortisol levels.
Hyperglycemia:
Hyperglycemia may result from various underlying health conditions that affect insulin production or utilization. Common causes include:
a. Diabetes: In diabetes, the pancreas does not produce enough insulin (type 1 diabetes), or the body's cells become resistant to insulin (type 2 diabetes), leading to elevated blood sugar levels.
b. Hormonal Imbalances: Hormonal imbalances, such as increased levels of cortisol, growth hormone, or glucagon, can contribute to insulin resistance and hyperglycemia.
c. Pancreatitis: Acute or chronic pancreatitis can impair the pancreas's ability to produce insulin, leading to hyperglycemia.
d. Cushing's Syndrome: Cushing's syndrome, a disorder characterized by excessive production of cortisol, can induce insulin resistance and hyperglycemia.
Medications and Treatments
Hypoglycemia:
Medications used to treat diabetes, such as insulin and certain oral medications (e.g., sulfonylureas, meglitinides), can lower blood sugar levels and increase the risk of hypoglycemia if not balanced with proper nutrition and monitoring. Additionally, other medications, such as beta-blockers and certain antibiotics, may also contribute to hypoglycemia.
Hyperglycemia:
Medications that may contribute to hyperglycemia include corticosteroids, antipsychotic medications, certain diuretics, and some antidepressants. Improper use or dosage adjustments of diabetes medications can also lead to hyperglycemia.
Lifestyle Factors
Hypoglycemia:
Lifestyle factors that may contribute to hypoglycemia include:
a. Skipping meals or inadequate food intake.
b. Excessive alcohol consumption, which can impair the liver's ability to release stored glucose.
c. Strenuous physical activity without proper carbohydrate intake.
Hyperglycemia:
Lifestyle factors that may contribute to hyperglycemia include:
a. Poor diet choices, such as excessive consumption of sugary or high-carbohydrate foods.
b. Sedentary lifestyle and lack of regular physical activity.
c. Stress and emotional factors can increase cortisol levels and contribute to insulin resistance.
How To Tell The Difference Between Hyperglycemia and Hypoglycemia?
Blood Sugar Levels
Hypoglycemia:
Hypoglycemia is characterized by blood sugar levels that fall below normal, typically below 70 milligrams per deciliter (mg/dL). Blood glucose monitoring is essential for confirming hypoglycemia, and prompt action is required to raise blood sugar levels to prevent complications.
Hyperglycemia:
Hyperglycemia is defined by blood sugar levels higher than normal, often exceeding 180 mg/dL. Monitoring blood sugar levels through regular glucose testing can help identify hyperglycemia and guide treatment and management strategies.
Symptoms and Warning Signs
Hypoglycemia:
Hypoglycemia often presents with a distinct set of symptoms that can vary in severity, including:
a. Shakiness or tremors
b. Sweating or clamminess
c. Palpitations or rapid heartbeat
d. Hunger or nausea
e. Confusion or difficulty concentrating
f. Irritability or mood changes
g. Headache or dizziness
h. Blurred vision
i. Weakness or fatigue
j. Severe symptoms may include seizures or loss of consciousness.
Hyperglycemia:
Hyperglycemia may manifest with symptoms such as:
a. Increased thirst
b. Frequent urination
c. Fatigue or weakness
d. Blurred vision
e. Dry mouth or dry skin
f. Headache
g. Nausea or vomiting
h. Slow wound healing
i. Recurrent infections, such as urinary tract infections or yeast infections
j. Hyperglycemic crises, such as diabetic ketoacidosis (DKA) or hyperosmolar hyperglycemic state (HHS), may present with more severe symptoms, including confusion, rapid breathing, fruity breath odor, and unconsciousness.
Diagnostic Tests
Hypoglycemia:
Diagnostic tests for hypoglycemia include blood glucose monitoring, which measures the current blood sugar level. In some cases, additional tests such as continuous glucose monitoring (CGM) or oral glucose tolerance tests (OGTT) may be performed to assess glucose tolerance and insulin response.
Hyperglycemia:
Diagnostic tests for hyperglycemia involve blood glucose monitoring to measure blood sugar levels. Hemoglobin A1c (HbA1c) testing measures average blood sugar levels over the past two to three months and is used to assess long-term glycemic control. Additionally, other tests, such as urine ketone testing, may be performed to evaluate for ketosis in cases of severe hyperglycemia.
What Are The Warning Signs Of Hypoglycemia?
Common Symptoms
Hypoglycemia can manifest with a range of symptoms, which may vary in severity and presentation. Common symptoms of hypoglycemia include:
a. Shakiness or tremors
b. Sweating or clamminess
c. Palpitations or rapid heartbeat
d. Hunger or nausea
e. Confusion or difficulty concentrating
f. Irritability or mood changes
g. Headache or dizziness
h. Blurred vision
i. Weakness or fatigue
Recognizing these symptoms is essential for prompt intervention and prevention of severe hypoglycemic events.
Severe Symptoms and Emergency Response
In some cases, hypoglycemia can progress to more severe symptoms, requiring immediate medical attention. Severe symptoms of hypoglycemia may include:
a. Seizures
b. Loss of consciousness
c. Inability to swallow
d. Confusion or disorientation
If left untreated, severe hypoglycemia can lead to coma or even death. In cases of severe hypoglycemia, emergency response measures may include administering fast-acting carbohydrates such as glucose tablets, fruit juice, or glucose gel, retesting blood sugar levels, and adjusting treatment as needed. Glucagon injections may also be administered to individuals who cannot consume oral carbohydrates.
Management and Prevention Strategies
Management and prevention strategies for hypoglycemia aim to maintain blood sugar levels within a safe range and prevent recurrent episodes. Strategies may include:
a. Regularly monitor blood sugar levels using a glucose meter or continuous glucose monitoring (CGM) system.
b. Consuming regular meals and snacks containing carbohydrates, protein, and healthy fats.
c. Adjusting medication doses, timing, or types under the guidance of a healthcare provider.
d. Carrying fast-acting carbohydrates to quickly treat hypoglycemic episodes, such as glucose tablets, fruit juice, or hard candy.
e. Educating family members, caregivers, and coworkers about the signs and treatment of hypoglycemia.
f. Avoiding excessive alcohol consumption, which can impair the body's ability to regulate blood sugar levels.
g. Engaging in regular physical activity but taking precautions to monitor blood sugar levels and adjust carbohydrate intake as needed.
h. Working closely with a healthcare team, including a diabetes educator or nutritionist, to develop an individualized management plan for hypoglycemia.
Conclusion
Recognizing and understanding the differences between hypoglycemia and hyperglycemia is crucial for individuals with diabetes and those at risk of blood sugar imbalances. While hypoglycemia is characterized by low blood sugar levels and may lead to immediate symptoms such as shakiness or confusion, hyperglycemia involves elevated blood sugar levels. It can manifest with increased thirst or fatigue. Prompt identification and appropriate management of these conditions are essential for preventing complications and maintaining overall health and well-being. By monitoring blood sugar levels regularly, recognizing warning signs, and implementing preventive strategies, individuals can effectively manage their condition and minimize the risk of adverse outcomes associated with hypoglycemia and hyperglycemia. Consulting with healthcare professionals and adhering to personalized treatment plans are integral to diabetes management, ensuring optimal blood sugar control and quality of life.


.webp)

.avif)