A significant portion of the population in the United States is affected by chronic wounds. According to various estimates, around 2% of the population in the US suffers from chronic wounds. With the rise in the aging population, the affected population is only expected to increase. Cardiovascular diseases are a significant risk factor for impaired wound healing. The burden of cardiovascular diseases is significant. According to the Centres for Disease Control (CDC), around 8% of individuals in the United States suffered from some form of cardiovascular disease in 2015-2016. Given the high burden of cardiovascular disease, it is important for podiatrists and wound cardiovascular specialists to understand the impact of cardiovascular disease on wound healing.
Normal Wound Healing Physiology
Before understanding the impact of cardiovascular disease on wounds, it is important to take into consideration the normal physiology of wound healing. Broadly speaking, four main stages are recognized in a normal wound healing process. These include:
- Homeostasis
- Inflammation
- Proliferation
- Repair/Remodeling
The first stage - homeostasis - involves the activation of the coagulation cascade due to tissue injury which leads to the formation of a fibrin mesh. This is followed by an influx of neutrophils at the wound site which marks the beginning of the inflammation phase. Inflammation appears clinically as swelling and redness at the site of injury. This stage is important for the removal of bacteria and other contaminants present at the wound site.
In the third stage called the 'proliferation phase', the process of tissue repair begins. This is characterized by the deposition of collagen and extracellular matrix. The migration of myofibroblasts also begins in this stage which later facilitates the contraction of the wound edges. Angiogenesis or the formation of new blood vessels occurs simultaneously during this stage. Blood vessels are essential for nutrient and oxygen delivery to the newly formed 'granulation tissue'. The final stage of wound healing is marked by the replacement of type III collagen with type I collagen. This increases the tensile strength of the wound. The wound can regain 80% of its pre-injury strength.
How Cardiovascular Disease Affects Wound Healing?
Cardiovascular diseases include the diseases of the heart and blood vessels. Examples are coronary artery disease (CAD), stroke, congestive cardiac failure, and peripheral vascular disease. In cardiovascular diseases, the normal functioning of the heart is disrupted which leads to decreased perfusion of the body. In congestive cardiac failure, for instance, the body is unable to pump sufficient blood which affects the blood supply to the body. As previously discussed, oxygen and nutrients delivery to the wound site is critical in improved healing outcomes. Therefore, patients with cardiovascular diseases have compromised blood supply which leads to delayed wound healing. Peripheral vascular disease (PVD) is the most commonly implicated cardiovascular disease in the pathogenesis of wound healing.
Impact of Peripheral Arterial Disease On Wound Healing
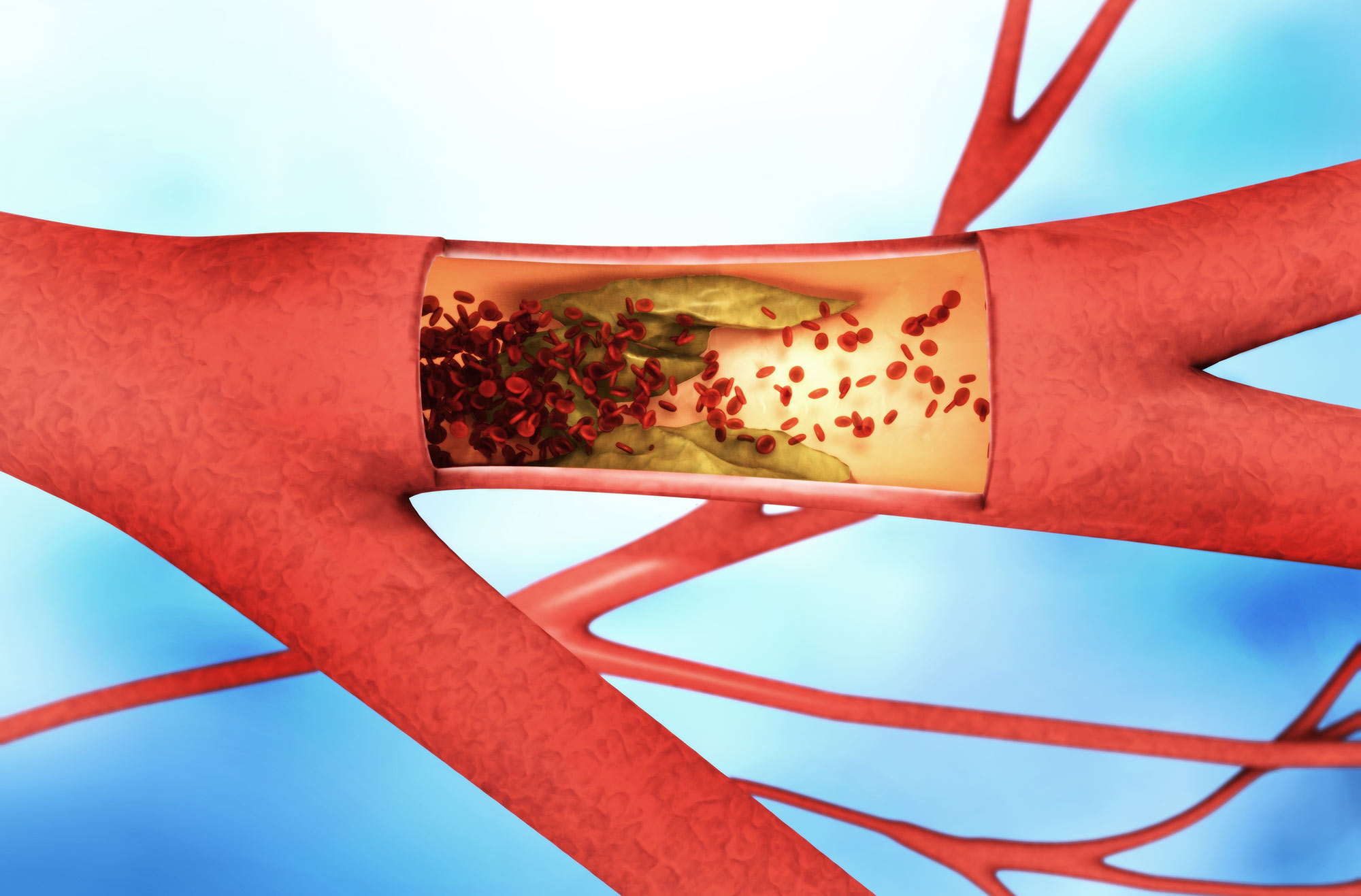
In the United States, appropriately 8 million people are reportedly suffering from peripheral vascular disease (PAD). The stenosis and narrowing of blood vessels due to atherosclerosis in the lower limbs leads to decreased blood flow. Due to compromised blood flow to the tissues, wound healing is delayed which leads to wound chronicity. Peripheral vascular disease is one of the leading causes of lower limb amputations. Therefore, early detection and screening of PAD are essential for limb salvage.
Peripheral vascular disease is usually asymptomatic at first and later progresses to intermittent claudication. Due to obstructed blood supply, tissue necrosis occurs in distal extremities which leads to the development of chronic, ischemic ulcers. These ulcers tend to be extremely painful, and are located on the tips of toes and sides of feet.
Ischemic ulcers have low tissue perfusion which favors bacterial colonization and contamination. The combination of hypoxia and infection halts the progression of normal wound healing which leads to tissue death. As a result, 66% of individuals undergo lower-limb amputations within the first 4 years of diagnosis. Given the high risk of lower limb amputation, early detection by podiatrists through regular screenings is critical. Wound care specialists can also provide specialized care to patients with ischemic ulcers that can help limit the progression of the disease.
Chronic wounds account for over $25 billion annual expenditure of healthcare in the United States. With the increase in the incidence of cardiovascular disease and chronic wounds, there is a need for early screening and prevention of cardiovascular diseases. Patients should be educated about the various risk factors that can lead to the development of cardiovascular disease. Smoking is a significant contributor to the development of many cardiovascular diseases. Therefore, health educational measures should be directed towards smoking cessation in at-risk individuals. Moderate physical exercise and other lifestyle modifications such as incorporating a balanced, healthy diet can lead to a significant reduction in cardiovascular risk factors.


.webp)

.avif)