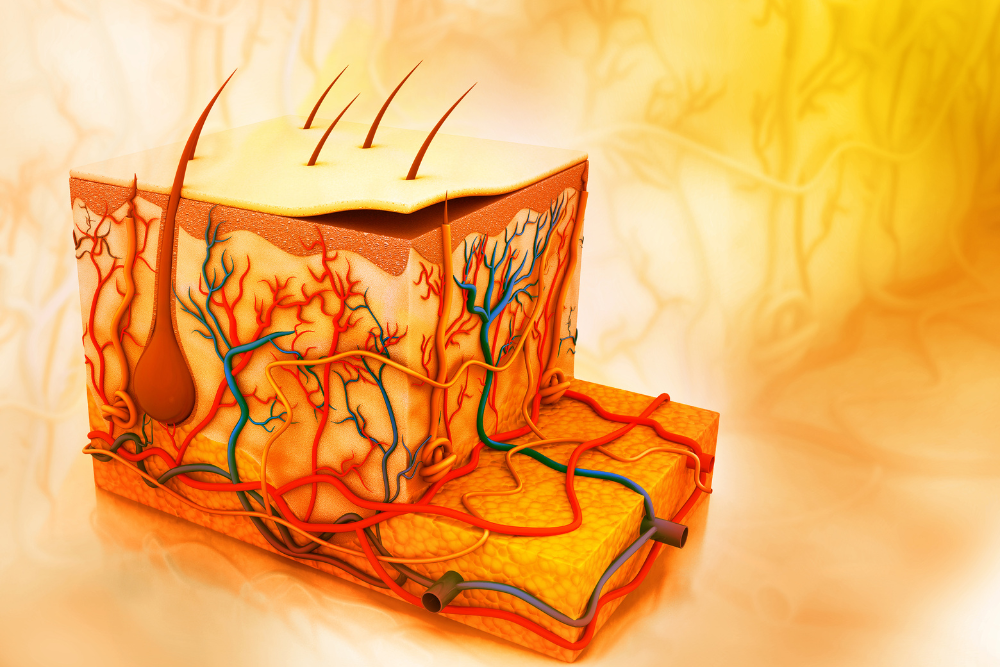
Skin anatomy
A wound is a disruption in the continuity of the epithelium of the skin. Therefore a proper understanding of skin anatomy and physiology can help wound care specialists and podiatrists better appreciate different aspects of wound healing related to the skin. The skin is the body's largest organ . It is readily visible, and therefore, skin problems have the potential to significantly impact patients’ perception of themselves and their psychological well-being.
Anatomy of The Skin
The human skin is divided into three main layers: the epidermis, dermis, and subcutaneous tissue. The dermis and epidermis are separated by a structure called the basement membrane. The thickness of skin varies depending on the location of the body and is primarily determined by the varying thickness of either the dermis or epidermis.
Epidermis
The epidermis is the avascular outermost layer of the skin. It is composed of keratinocytes and dendritic cells. Keratinocytes are the predominant cell type found in the epidermis, accounting for over 90% of all cells in the epidermis. They play an important role in the function of the skin as a protective barrier and through epithelization, restore the integrity of the skin during wound healing. Dendritic cells, on the other hand, play an important role in the immune system.
The epidermis is further subdivided into five layers. These skin anatomy layers are as follows: stratum corneum, stratum lucidum, stratum granulosum, stratum spinosum, and stratum basale.
- Stratum Corneum: It is the topmost layer of the epidermis. Stratum corneum is composed of flattened, anucleated cells called “keratinocytes”. These cells are filled with a tough, fibrous, insoluble protein called keratin, hence the name. The presence of keratin and other proteins in the stratum corneum confers it the ability to withstand abrasion. Stratum corneum accounts for about two-thirds of the thickness of the epidermis. The thickness of the stratum corneum varies depending on characteristics such as age and gender. Stratum corneum is enriched with a lipid matrix which enhances the protective barrier function of the skin.
- Stratum Lucidum: Beneath the stratum corneum, there is usually a second upper layer of skin called the "stratum lucidum". Unlike other layers of the epidermis, it is only present in areas of thickened skin such as palms and soles. It is absent from areas of thinner skin such as the eyelids. Under a microscope, stratum lucidum appears as a thin, translucent layer of flattened keratinocytes.
- Stratum Granulosum: The stratum granulosum is also known as the "granular layer" because of the presence of granules in the keratinocytes of this layer. Unlike the first two layers of the epidermis, the keratinocytes have not yet been flattened and have a characteristic diamond shape. Stratum granulosum is also the layer in which the process of keratinization begins.
- Stratum Spinosum: The stratum spinosum gets its name from the spine like projections of keratinocytes in this layer. However, these spines do not exist in living cells and are only created as artifacts during tissue preparation. The keratinocytes in this layer are held together by desmosomes or "tight junctions''. So when the cytoplasm of keratinocytes shrinks during tissue preparation, the desmosomes take on the appearance of a "spine".
- Stratum Basale: The stratum basale is the innermost or basal layer of the epidermis. The cells in this layer are mitotically active and give rise to new keratinocytes pushed toward the epidermis's upper layers. Melanocytes, the pigment-producing cells of the skin, are also present in this layer.
Dermis
The dermis is the thickest, vascular layer of the skin. Unlike the epidermis which contains keratinocytes, the dermis is populated with fibroblasts and contains vasculature and innervation of the skin. The thickness of the dermis varies depending on the location of the body which also results in differences in the thickness of the skin. The blood vessels in the dermis are responsible for maintaining homeostasis, providing nutritional support, and thermoregulation. Even though the blood vessels do not enter into the epidermis, the cells of the epidermis derived their oxygen and nutrients brought by the vasculature in the dermis through simple diffusion.
The dermis has two layers: the thin outer layer called the “papillary dermis” and a deeper thick layer called the “reticular dermis”. Indenting into the overlying epidermis, there are peg-like projections on the outer surface of the papillary dermis called “dermal papillae”. Dermal papillae might contain blood vessels, free nerve endings, and touch receptors.
The reticular dermis, unlike the papillary dermis which contains loose areolar tissue, contains dense connective tissue. It contains thick bundles of collagen fibers and accounts for over 80% of the total thickness of the dermis. Unlike the epidermis and dermis which are separated by a basement membrane, there is no clear demarcation between the papillary and reticular dermis.
Hypodermis
The hypodermis, or the subcutaneous tissue, is the bottom-most layer of skin and lies just below the dermis. It is primarily composed of adipose tissue and helps to attach the dermis to the underlying structures where the hair follicles lie. The hypodermis acts as an insulator, and an energy reservoir, and provides cushioning to the skin.
Functions of the Skin
Skin is one of the largest, visible organs in the human body. Several medical conditions can have cutaneous manifestations and can provide clinicians with an important clue regarding their diagnosis. Skin performs several important functions for the human body. An understanding and appreciation of these functions can help clinicians better address the impact of skin pathologies.
- Protection: Arguably one of the most important functions performed by the skin is the protection of internal organs against external pathogens, environmental agents, and UV radiation. It serves as a protective barrier to the human body. The first line of defense against the entry of pathogens into the human body is an intact epithelium. Sebum, which is a lipid oily substance secreted by the sebaceous glands on the skin, provides an acidic coating that confers it with antibacterial properties. The pigment melanin which contributes to skin pigmentation helps to protect against the harmful UV rays of the sun. In addition, the skin also has immune cells like the Langerhan cells and tissue macrophages.
- Thermoregulation: Skin plays an important role in maintaining body temperature through a process called thermoregulation. The two primary mechanisms involved in thermoregulation are sweating and blood circulation. To dissipate excess heat, the blood vessels in the skin dilate which results in increased blood flow. The heat is lost from the surface of the skin by conduction, convection, radiation, and evaporation. Excess amount of sweat is also produced by the sweat glands which results in the dissipation of heat. In contrast, vasoconstriction of the blood vessels results in the conservation of heat.
- Sensation: Several receptors are present on the skin to detect sensations like pain, touch, temperature, and pressure. These sensations are then carried by nerve fibers to the cerebral cortex where they are interpreted. Some examples of sensory receptors present on the skin include Meissner corpuscles, Merkel cells, Krause end bulbs, and unmyelinated free nerve endings. The importance of skin sensation can be demonstrated by the fact that people with diabetic neuropathies have an increased risk of trauma. Skin sensations are an adapter response to protect the body against external trauma.
- Metabolism: The skin is an important site for the synthesis of vitamin D in the presence of sunlight. In the presence of UV light, 7-dehydrocholesterol is converted to cholecalciferol. Vitamin D plays an important role in the regulation of calcium and phosphorus levels in the body. The deficiency of vitamin D can result in thin, brittle bones. This is why adequate sun exposure is often recommended for optimal vitamin D synthesis.


.webp)

.avif)