Debridement is a critical component of wound care that involves the removal of necrotic tissue and debris from the wound. In patients with no significant comorbidities, natural debridement and sloughing of dying tissue keep pace with the normal wound healing process. However, people with poor nutrition, multiple comorbidities, diabetes require intervention by podiatrists and wound care specialists for better wound healing. Serial debridements help to restore a functional wound healing environment that helps to accelerate healing. [1]
Role of Debridement In Wound Healing
The wound healing process is a finely tuned sequential event that involves the interaction of various cytokines and stimulators that are produced by the body. [2] The presence of necrotic or debris in the wound bed is an impediment to wound healing as it affects the migration and multiplication of cells. It also prolongs inflammation by excessive production of proinflammatory cytokines which further delays wound healing. [3] In addition, necrotic tissue is susceptible to bacterial contamination and infection which can further spread to deeper tissues leading to cellulitis, osteomyelitis, sepsis, amputation, and even death. Necrotic tissue has a poor blood supply which further contributes to wound chronicity. [4]
Wound debridement helps to convert a chronic wound into an “active wound” and facilitates wound healing through the following mechanisms:
- Reduced Bacterial Burden: Necrotic tissue is a nidus for bacterial contamination. [5] Through the removal of devitalized tissue, debridement helps to reduce bacterial load in the wound bed which helps to accelerate the wound healing process.
- Improved Tissue Perfusion: Removal of necrotic, dead tissue helps to restore perfusion to the wound site which improves oxygen delivery to the wound bed. An adequate supply of oxygen is vital for the healing process, and therefore, debridement helps to improve healing through restoration of local blood supply.
- Migration of Fibroblasts: Bacteria compete with normal tissue for the supply of nutrients and energy. This in turn compromises the migration of fibroblasts into the extracellular matrix which is essential for wound healing to occur. A clean, debrided wound can recruit fibroblasts to the wound site which lays down collagen fibrils. This helps to fill up the epithelial defect caused by the wound. [6]
- Better Visualisation of Wound Bed: Debridement allows wound care specialists and podiatrists better visualization of the viable tissue in wound bed which can help them plan appropriate wound care accordingly.
Methods of Wound Debridement
Wound debridement is a critical component of wound care as it accelerates the wound healing process. The following methods of wound debridement are currently available:
- Surgical Debridement: It involves the removal of necrotic or dead tissue with the help of a sharp surgical instrument like a scissor or a scalpel. It is indicated whenever there is a need of removing large areas of necrotic tissue, and in presence of infection. Surgical debridement has been found to improve wound re-epithelialization and contraction. [7] It also decreases bacterial load in the wound bed. However, this method requires surgical training and expertise.
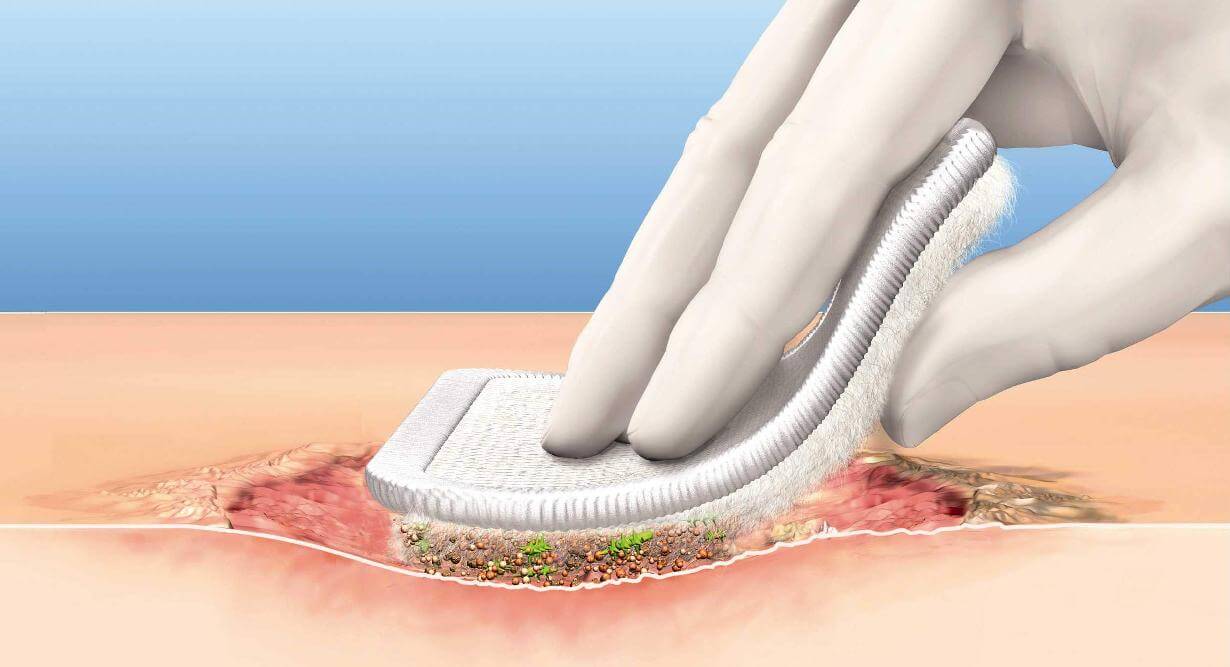
- Mechanical Debridement: It involves the use of wet or dry dressings for the removal of superficial layers of dead, necrotic tissue. The drawback of using this method is that it might also remove viable tissue which makes it non-selective. Furthermore, it is a painful procedure and as patients value comfort over healing, it might not be a feasible method. [8]
- Autolytic Debridement: Autolytic debridement is the use of the body's enzymatic system for the removal of devitalized tissue. As these enzymes function best in a moist wound environment, this method requires the use of moisture-retaining wound dressings. Compared to other methods, it is relatively slow but is generally considered to be a safe method. [9]
- Enzymatic Debridement: It involves the topical application of enzymes such as collagenase to the necrotic tissue. These enzymes dissolve and break down the necrotic tissue, thereby removing the devitalized tissue from the wound bed. [10] It is generally considered to be a safe method but should be avoided in patients who have allergies to the component of enzyme preparation.
- Maggot Therapy: This method involves the use of sterile maggots for the dissolution of necrotic tissue. Proteolytic enzymes present in the saliva of maggots dissolve and break down the necrotic tissue, and leave the healthy, viable tissue behind. This method can be used in the treatment of pressure ulcers, diabetic foot ulcers, venous ulcers, and other types of chronic wounds. Maggot therapy improves wound healing and can be used for the debridement of wounds when surgical methods are not applicable. However, a negative reaction to the use of maggots and discomfort can limit its use. [11]
References:
- Cardinal M, Eisenbud DE, Armstrong DG, Zelen C, Driver V, Attinger C, Phillips T, Harding K. Serial surgical debridement: a retrospective study on clinical outcomes in chronic lower extremity wounds. Wound Repair and Regeneration. 2009 May;17(3):306-11.
- Hopkinson I. Molecular components of the extracellular matrix. Journal of wound care. 1992 May 2;1(1):52-4.
- Young T. Reviewing best practice in wound debridement. Practice Nursing. 2011 Sep;22(9):488-92.
- Ayello EA, Cuddigan J, Kerstein MD. Skip the knife: debriding wounds without surgery. Nursing2020. 2002 Sep 1;32(9):58-64.
- Schultz GS, Sibbald RG, Falanga V, Ayello EA, Dowsett C, Harding K, Romanelli M, Stacey MC, Teot L, Vanscheidt W. Wound bed preparation: a systematic approach to wound management. Wound repair and regeneration. 2003 Mar;11:S1-28.
- Wysocki AB. Wound fluids and the pathogenesis of chronic wounds. Journal of WOCN. 1996 Nov 1;23(6):283-90.
- Brem H, Stojadinovic O, Diegelmann RF, Entero H, Lee B, Pastar I, Golinko M, Rosenberg H, Tomic-Canic M. Molecular markers in patients with chronic wounds to guide surgical debridement. Molecular medicine. 2007 Jan;13(1):30-9.
- Vermeulen H, Ubbink DT, De Zwart F, Goossens A, De Vos R. Preferences of patients, doctors, and nurses regarding wound dressing characteristics: a conjoint analysis. Wound repair and regeneration. 2007 May;15(3):302-7.
- Young T. Skin failure and wound debridement. Nurs Resid Care [Internet]. 2012;14(2):74–9. Available from: http://dx.doi.org/10.12968/nrec.2012.14.2.74
- Hart J. Inflammation 1: its role in the healing of acute wounds. Journal of wound care. 2002 Jun;11(6):205-9.
- Steenvoorde P, Budding T, Oskam J. Determining pain levels in patients treated with maggot debridement therapy. Journal of wound care. 2005 Nov;14(10):485-8.


.webp)

.avif)