Draining sanguineous fluid from chest tubes requires understanding of fluid properties and knowing how tubes function. Sterilized equipment, such as Chest Drainage Systems, and protective gear are crucial for this procedure.
Techniques that prove effective include proper positioning of patients, inserting the tube correctly, and utilizing a sealed draining device. One must ensure a sterile environment for safety, vigilant management of complications, and quick action during emergencies.
After draining, it's important to check vital signs, take care of the wound, and inform patients about their medication and potential signs of complications.
Key Takeaways
- Proper positioning of patients and accurate chest tube placement are crucial for effective drainage.
- Regular checks of the closed drainage device's efficiency are critical when linked with the chest tube.
- Utilizing sterile methods, wearing protective attire, and ensuring rapid response to emergencies can prevent infections and manage unexpected issues.
- Post-drainage monitoring of vital signs, with particular focus on oxygen saturation levels, allows us to judge the success of the treatment.
- Optimal recovery involves focusing on wound maintenance, educating patients about their medication and signs of complications, as well as immediate reporting of any inflammation.

The Dangers of Sanguineous Fluid And Chest Tubes
Sanguineous fluid, a term often encountered in medical practice, describes drainage filled with blood. This fluid typically arises following surgery or trauma, containing a mix of blood and serous fluid. Careful attention is crucial for managing this fluid and preventing complications.
On another note, chest tubes play an essential role in managing sanguineous fluid. These tubes serve as channels for the evacuation of accumulated fluids or air from the pleural space, which reestablishes negative intrapleural pressure and enables full lung expansion. Conditions such as pneumothorax, hemothorax, pleural effusion, and postoperative care often necessitate the use of chest tubes.
Proficient management of sanguineous fluid via chest tubes hinges on understanding the fluid's properties and the tube's function. This understanding is key to guiding healthcare professionals in delivering optimal patient care, anticipating potential complications, and planning suitable interventions.
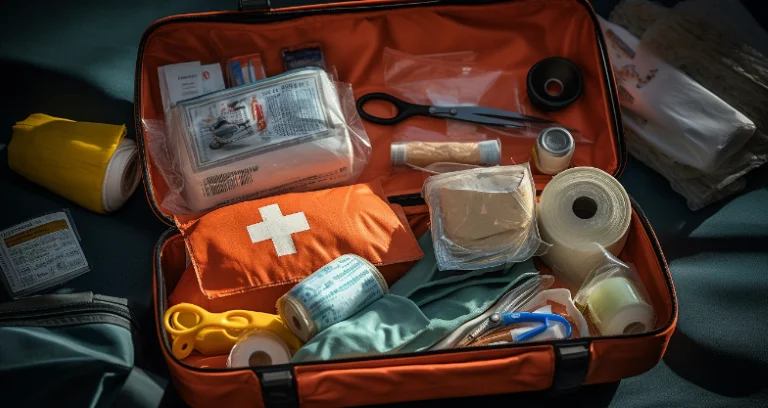
Essential Equipment for Fluid Drainage
Draining sanguineous fluid with chest tubes necessitates specific equipment. These tools enhance drainage efficiency and patient safety.
Critical equipment for fluid drainage comprises:
- Chest Drainage System: A closed system for draining fluid from a patient's chest, maintaining a sterile environment to prevent infections.
- Measurement Device: Quantifies the amount of drained fluid, supporting patient monitoring and treatment assessment.
- Protective Gear: Gloves, gowns, eye protection safeguard healthcare professionals from potential exposure to infectious fluids.
Maintaining this equipment is crucial to ensure functionality and reliability. Regular sterilization of reusable items, replacement of disposable ones, appropriate storage to keep their integrity, and prompt inspection and repair of faulty equipment are all part of this process.
Step-by-Step Guide to Draining Techniques
Eliminating sanguineous fluid requires a precise, step-by-step process that clinicians must adhere to for safeguarding patients and ensuring successful treatment. Comprehending fluid dynamics combined with correct placement of the tube is vital for efficient drainage and patient ease.
To start, position the patient appropriately, ideally at a 30-45 degree angle to take advantage of gravity-assisted drainage. Next, insert a chest tube into the pleural space, paying careful attention to its location. With correct positioning, fluid dynamics aid the drainage procedure. Connect this tube subsequently to a closed drainage apparatus.
This apparatus, typically having three chambers, facilitates the collection, measurement, and disposal of fluid while maintaining unidirectional flow, a crucial element for sustaining negative pressure within the pleural space.
Comfort for the patient remains a significant concern throughout the process. Appropriate pain relief, secure tube placement, and frequent checks for potential issues such as infection or displacement of the tube can greatly improve ease for the patient.
Safety Precautions During Drainage Procedure
Implementing safety measures during a drainage procedure is as crucial as following the procedural steps. One must adhere to these precautions to avoid complications and ensure patient well being.
Keeping everything clean stands as a fundamental principle in infection prevention. Sterilize everything as they minimize the risk of bacterial introduction into the patient's body. Essential elements include wearing protective clothing, using sterile gloves, and meticulously disinfecting equipment.
Effective response to emergencies is another safety consideration. Medical teams must remain alert to signs of distress or sudden changes in the patient's condition. Quick, coordinated actions can help alleviate any adverse outcomes.
To sum up, these points are vital:
- Sterile techniques for infection prevention.
- Quick emergency response capability.
- Vigilant complications management.

Post-Drainage Patient Care and Monitoring
Post-drainage care and consistent observation are imperative following chest tube sanguineous fluid drainage. Monitoring vital signs forms the first step, particularly focusing on oxygen saturation levels, respiratory rates, and blood pressure. Should notable changes occur, immediate medical action is required.
Care for the wound is another paramount aspect. Keeping the site clean along with dryness helps infection prevention. Immediate reporting of inflammation signs, such as redness, warmth, or pus discharge, to healthcare providers is necessary.
Educating the patient contributes substantially to optimal recovery. Instructions on medication regimen adherence, adequate rest necessity, and complication signs to monitor are key. Advice on avoiding strenuous activities that could disrupt healing is also crucial.
Lastly, follow-up checks are essential in care after the procedure. These visits enable healthcare workers to evaluate patient progress, respond to concerns, and modify treatment strategies as needed.
Frequently Asked Questions
What are the nursing interventions for a patient with a chest tube?
Nursing interventions for a patient with a chest tube include monitoring the patient's respiratory status and vital signs, assessing the chest tube insertion site for signs of infection or complications, providing pain management, assisting with mobility and activities of daily living, educating the patient and family about the chest tube and its care, and maintaining a sterile technique when handling the chest tube and drainage system.
How to troubleshoot a chest tube drainage system?
To troubleshoot a chest tube drainage system, the nurse should first assess the patient's condition and vital signs, check for any kinks or obstructions in the tubing, ensure the drainage system is below the level of the patient's chest, check for leaks in the system, assess the dressing site for any signs of infection, and if any issues persist, promptly notify the healthcare provider for further evaluation and intervention.
What steps should you take to ensure that the chest tube drainage system is functioning properly?
To ensure that the chest tube drainage system is functioning properly, the nurse should regularly assess the chest tube insertion site for signs of infection, ensure that the drainage system is below the level of the patient's chest, monitor the amount and color of drainage in the collection chamber, and make sure that the water seal is intact and at the correct level. Any sudden increase in drainage, bubbling in the water seal chamber, or disconnection of the tubing should be promptly addressed.
Which action would the nurse immediately take if a chest tube is dislodged completely?
If a chest tube is dislodged completely, the nurse should immediately apply an occlusive dressing over the insertion site to prevent air from entering the pleural space. This will help maintain the patient's respiratory status while awaiting further medical intervention. The nurse should also closely monitor the patient for signs of respiratory distress and notify the healthcare provider promptly.
What should the nurse ensure when using the water seal chest tube drainage?
When using a water seal chest tube drainage system, the nurse should ensure that the water seal chamber is filled with the prescribed amount of sterile water to the correct level indicated by the manufacturer. It is important to monitor for continuous bubbling in the water seal chamber, as this can indicate an air leak. The nurse should also ensure that the chest tube is securely taped to prevent accidental dislodgement.
Which actions, when taken by the nurse, can prevent chest tube occlusions?
To prevent chest tube occlusions, the nurse should ensure that the drainage system is kept below the level of the patient's chest at all times to facilitate proper drainage. Regularly milk or strip the tubing as ordered to prevent clot formation and maintain patency. Encouraging the patient to cough and deep breathe can also help prevent stagnant fluid or blood from obstructing the tubing.
What is the nurse's priority action if the client's chest tube falls out of the chest?
The nurse's priority action if the client's chest tube falls out of the chest is to immediately apply an occlusive dressing over the insertion site to prevent air from entering the pleural space. This will help prevent a pneumothorax and maintain the patient's respiratory status. The nurse should then notify the healthcare provider promptly for further instructions on reinserting the chest tube.
What is the method of removing fluid from the chest pleural effusion?
The method of removing fluid from the chest pleural effusion is through a procedure called Thoracentesis. During this procedure, a needle or catheter is inserted through the chest wall into the pleural space to drain fluid. The fluid is then collected in a sterile container for analysis. This procedure is typically performed under ultrasound guidance to ensure accuracy and safety.

The Wound Pros
4640 Admiralty Way, Marina Del Rey, CA 90292
(888) 880-3451
https://maps.app.goo.gl/oW3wtEt5njnkRiNV6



.webp)

.avif)