Wound care is a pivotal domain within healthcare, addressing injuries that range from minor cuts to complex surgical incisions. Wound management's intricacies go beyond physical healing, delving into the physiological nuances that dictate recovery. One crucial factor that significantly influences the wound-healing process is the concept of aging.
As we age, our bodies undergo a myriad of changes that extend beyond the surface, impacting the core of wound healing mechanisms. This blog will delve into the profound implications of aging in wound care and how age affects the progress of wound growth, mainly focusing on issues such as pressure ulcers on aging skin and specialized wound care for the elderly.
Understanding the Concept of Aging in Wound Care
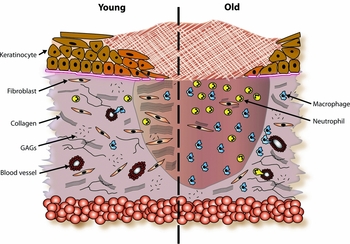
Aging skin transforms over time, affecting wound healing intricacies. Thinning of the skin layers and reduced collagen production result in decreased elasticity, making aged skin more vulnerable to injuries. Immune response changes with age, leading to delayed inflammation and extended healing phases.
Pressure ulcers are a significant concern in aging individuals. Prolonged pressure on specific body areas and reduced skin resilience create an environment conducive to ulcer formation. These ulcers demand specialized attention due to the unique needs of elderly skin.
Recognizing the impact of aging on wound care is essential. Aging isn't just a number; it's a critical factor influencing treatment outcomes. By comprehending the shifts in aging skin and complications like pressure ulcers, we pave the way for more effective wound management. The following sections delve into how these insights reshape clinical treatments and address challenges and opportunities in wound care for the elderly.
Impact on Clinical Treatment
The effect of aging on wound healing has profound implications for clinical treatment strategies. In elderly individuals, the wound-healing process tends to be slower and more intricate. The inflammatory response, a crucial initial stage of healing, is often delayed in aging skin. This delay can lead to a prolonged inflammatory phase, affecting the subsequent proliferation and remodeling stages.
The extended healing phases in aging individuals also make them more susceptible to chronic wounds. Conditions like pressure ulcers, diabetic ulcers, and venous stasis ulcers become more prevalent due to decreased skin resilience and impaired blood circulation. These chronic wounds demand vigilant management, as their persistent nature can lead to severe complications.
To address these challenges, personalized treatment plans for elderly patients are paramount. Tailoring wound dressings and therapies to accommodate the characteristics of aging skin can significantly improve outcomes. Additionally, addressing underlying health conditions that might hinder the healing process is essential in achieving successful wound closure.
Challenges in Wound Management
Wound management for aging individuals comes with its challenges, primarily rooted in the unique characteristics of aging skin. The increased vulnerability to infections is a critical concern. Aging skin exhibits reduced antimicrobial activity and impaired barrier function, creating an environment conducive to microbial invasion. This susceptibility calls for meticulous wound hygiene and preventive measures to avert infections.
Pain management also poses a complex challenge in wound care for the elderly. Sensory changes associated with aging can affect pain perception, making pain assessment and relief strategies intricate. Balancing effective pain control with the primary goal of wound healing becomes a delicate task.
Moreover, chronic wounds can have a significant psychological impact on aging individuals. The prolonged healing journey can lead to frustration, isolation, and depression. Addressing the psychological aspects of wound care is thus a crucial component of holistic wound management.
Understanding and mitigating these challenges become imperative as we navigate the intricate landscape of wound care for the aging population. Tailored wound management strategies that account for the vulnerabilities of aging skin and address both physical and psychological well-being are essential for promoting optimal healing outcomes. In the subsequent sections, we explore strategies and advancements that offer promising solutions in geriatric wound care.
Strategies for Optimal Wound Care in Aging Patients
Navigating the complexities of wound care for aging patients necessitates a comprehensive approach. Beginning with a thorough wound assessment, healthcare professionals must evaluate the wound, surrounding skin, and potential underlying health conditions. This holistic assessment forms the foundation for devising personalized treatment plans that accommodate the specific needs of aging skin.
Utilizing advanced wound care products is another critical strategy. Moisture-retentive dressings help maintain the optimal wound environment, preventing excessive dryness or moisture. Growth factors and bioactive compounds can stimulate healing, addressing the delayed phases of wound closure that often accompany aging skin.
Collaboration among various healthcare disciplines is paramount in optimizing wound care for the elderly. A multidisciplinary approach that involves wound care specialists, geriatricians, nurses, and nutritionists ensures that all aspects of a patient's well-being are considered. Addressing nutritional needs, mobility issues, and comorbidities contributes to a more comprehensive and effective treatment plan.
Future Directions and Research
Geriatric wound care is rapidly evolving, driven by emerging technologies and a growing understanding of aging-related physiological changes.
Preventative strategies also warrant attention in geriatric wound care. Education for caregivers and aging individuals alike can empower them with the knowledge to mitigate wound risks. Lifestyle modifications, including maintaining proper nutrition, staying hydrated, and engaging in physical activity, are pivotal in supporting skin health and averting chronic wounds.
Conclusion
In the intricate interplay between aging and wound care, it's clear that age is not just a number—it's a critical determinant of treatment success. Understanding how aging impacts wound healing processes, particularly in the context of pressure ulcers and other challenges, allows healthcare providers to tailor treatments to the unique needs of aging skin.
As we conclude this exploration, it's evident that effective wound care for the elderly necessitates a multifaceted approach. By comprehensively assessing wounds, utilizing advanced products, and fostering collaboration across healthcare disciplines, we can improve outcomes and elevate the quality of life for aging individuals. Embracing emerging technologies and adopting preventative strategies will further contribute to the ongoing evolution of geriatric wound care. Through these efforts, we can ensure that the aging population receives the specialized care they deserve, optimizing their wound-healing journey and overall well-being.


.webp)

.avif)