Fournier's gangrene is a rare but life-threatening bacterial infection that primarily affects the genital, perineal, and perianal regions. This condition is characterized by rapid tissue destruction, severe pain, and systemic toxicity, often requiring urgent medical intervention. Understanding Fournier's gangrene is crucial due to its rapid progression and high mortality rate if not treated promptly.
What is Fournier's Gangrene?
Fournier's gangrene is a severe, rapidly progressing infection of the soft tissues, primarily affecting the genital, perineal, and perianal areas. This condition involves necrotizing fasciitis, where bacteria invade the fascial planes and subcutaneous tissue, leading to widespread tissue death and systemic toxicity. The infection is typically polymicrobial, involving a mixture of aerobic and anaerobic bacteria.
Historical Background
Fournier's gangrene was first described in 1883 by French venereologist Jean Alfred Fournier, who documented a series of cases involving the rapid onset of gangrene in young men without any apparent cause. Since then, our understanding of the disease has evolved significantly. It is now recognized that Fournier's gangrene can affect individuals of any age and gender, often linked to underlying conditions such as diabetes, immune suppression, or trauma to the affected area.
How it Specifically Affects the Body
Fournier's gangrene begins with an infection in the genital or perianal region, often following minor trauma, surgical procedures, or infections. The bacteria release toxins that cause tissue death and spread rapidly along the fascial planes. The condition is marked by severe pain, swelling, and erythema in the affected area. As the infection progresses, skin discoloration occurs, turning red, purple, or black as tissues die.
The systemic impact of Fournier's gangrene is profound. Patients often experience fever, malaise, and signs of sepsis, including low blood pressure and altered mental status. Without prompt and aggressive treatment, the infection can spread to adjacent areas, leading to extensive tissue destruction, multiple organ failure, and death.
Causes and Risk Factors
Common Causes of Fournier's Gangrene
Fournier's gangrene is primarily caused by a polymicrobial infection involving both aerobic and anaerobic bacteria. Common bacterial species implicated include Escherichia coli, Klebsiella, Streptococcus, Staphylococcus, and various anaerobes such as Bacteroides and Clostridium. These bacteria typically enter the body through a breach in the skin, such as a cut, surgical wound, or skin ulcer. The infection rapidly progresses due to the synergy between these bacteria, which produce toxins and enzymes that destroy tissue and impede blood flow, leading to necrosis.
Risk Factors
Diabetes
Diabetes is one of the most significant risk factors for Fournier's gangrene. High blood sugar levels can impair the immune system, reducing the body's ability to fight infections. Additionally, diabetes often leads to poor blood circulation and nerve damage, particularly in the lower extremities, which can delay the detection and treatment of wounds and infections. Diabetic patients are more prone to developing skin ulcers and infections that can escalate to Fournier's gangrene if not managed promptly.
Immune System Deficiencies
Individuals with compromised immune systems are at a higher risk of developing Fournier's gangrene. This includes patients with conditions such as HIV/AIDS, those undergoing chemotherapy, and those on immunosuppressive medications for autoimmune diseases or after organ transplants. A weakened immune response can allow bacteria to proliferate unchecked, increasing the likelihood of severe infections like Fournier's gangrene.
Recent Surgeries or Injuries in the Genital or Perineal Area
Surgical procedures and traumatic injuries in the genital or perineal region can create an entry point for bacteria, setting the stage for infection. Surgical wounds, especially those not kept clean or that heal poorly are susceptible to bacterial colonization. Additionally, injuries such as cuts, abrasions, or puncture wounds in these areas can similarly predispose individuals to Fournier's gangrene if bacteria are introduced and allowed to thrive.
Other Contributing Factors
Obesity: Excess body weight can lead to poor wound healing and increased risk of infections due to skin folds and difficulty maintaining proper hygiene.
Alcohol Abuse: Chronic alcohol consumption can impair liver function and the immune system, making the body more susceptible to severe infections.
Chronic Kidney Disease: Patients with kidney disease often have compromised immune function and poor wound healing capabilities, heightening the risk of infections.
Malnutrition: Poor nutritional status can weaken the immune system and impair wound healing, making individuals more vulnerable to infections.
Fournier's Gangrene Symptoms
Early Signs and Symptoms
Early detection of Fournier's gangrene is critical for effective treatment and improved outcomes. The initial signs can be subtle and resemble other less severe conditions, often leading to medical attention delays. Early symptoms include:
Pain and Tenderness: The first and most common symptom is sudden, severe pain in the genital, perineal, or lower abdominal areas. This pain is typically disproportionate to any visible signs of infection.
Swelling and Redness: The affected area may become swollen and red. As the infection spreads, the skin may become shiny and tense.
Fever: A mild fever might accompany these early symptoms as the body attempts to fight the infection.
Progression of Symptoms
As Fournier's gangrene progresses, the infection rapidly spreads, and the symptoms become more pronounced and severe. This stage is marked by:
Increased Swelling and Pain: The swelling and pain intensify, often excruciating and unresponsive to over-the-counter pain relief.
Skin Changes: As necrosis sets in, the skin may change color, turning dusky, purplish, or dark red. Blisters and bullae filled with fluid or pus may develop on the surface.
Foul-Smelling Discharge: A hallmark sign of Fournier's gangrene is a foul-smelling discharge emanating from the infected area. This discharge is often the result of tissue breakdown and the release of toxins by the bacteria.
Gas Formation: Subcutaneous gas production by anaerobic bacteria can cause a crackling sensation under the skin, known as crepitus. This is a critical sign of rapidly advancing infection.
Severe Symptoms Indicating Advanced Stages
In the advanced stages, Fournier's gangrene can lead to systemic symptoms that indicate a severe, life-threatening condition. These include:
Sepsis: As the infection enters the bloodstream, patients may exhibit signs of sepsis, including high fever, rapid heart rate, rapid breathing, and confusion. Sepsis is a medical emergency requiring immediate intervention.
Severe Necrosis: Extensive tissue death and blackened skin are visible. The necrotic tissue may begin to slough off, revealing underlying muscle and fat.
Shock: Patients may go into septic shock, characterized by dangerously low blood pressure, leading to organ failure and potentially death if not treated promptly.
How to Differentiate from Other Conditions
Differentiating Fournier's gangrene from other conditions with similar symptoms is crucial for timely treatment. Conditions that might be confused with Fournier's gangrene include:
Cellulitis: Unlike Fournier's gangrene, cellulitis typically involves more superficial layers of the skin and does not produce gas or extensive necrosis.
Epididymitis or Orchitis: These conditions involve infection and inflammation of the epididymis or testes, causing scrotal pain and swelling but not the severe necrosis and systemic symptoms of Fournier's gangrene.
Hernia: Inguinal hernias can cause pain and swelling in the groin area but are distinguishable through imaging studies and the absence of infection signs.
Fournier's gangrene is a medical emergency requiring immediate recognition and aggressive treatment. Awareness of its symptoms, especially the early signs and rapid progression, can significantly enhance patient outcomes through prompt medical intervention.
Diagnosis
Diagnosing Fournier's gangrene promptly is essential due to the rapid progression and high mortality rate associated with the condition. The diagnostic process involves a combination of medical history, physical examination, imaging studies, and laboratory tests to confirm the presence and extent of the infection.
Medical History and Physical Examination
The initial step in diagnosing Fournier's gangrene is a thorough medical history and physical examination. During this phase, the healthcare provider will:
Medical History: Ask about the onset and duration of symptoms, including pain, swelling, and any recent injuries or surgeries in the genital or perineal area. The patient’s medical history will also be reviewed for underlying conditions such as diabetes, immune system deficiencies, or other factors that could predispose them to infections.
Physical Examination: The provider will thoroughly examine the affected area. They will look for signs of infection, such as redness, swelling, skin discoloration, and blisters or necrotic tissue. The characteristic foul-smelling discharge and subcutaneous gas (crepitus) are critical indicators of Fournier's gangrene.
Imaging Studies
Imaging studies play a crucial role in confirming the diagnosis and assessing the extent of the infection. The most commonly used imaging modalities include:
MRI (Magnetic Resonance Imaging): MRI provides detailed images of soft tissues, which can help identify the spread of infection, the presence of gas in tissues, and the extent of necrosis. It is particularly useful in differentiating Fournier's gangrene from other conditions.
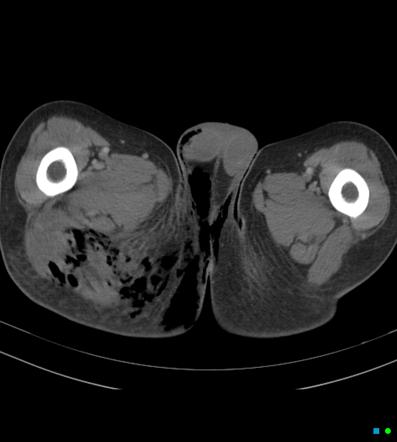
CT Scans (Computed Tomography): CT scans effectively detect gas formation and the spread of infection into deeper tissues. They offer a quicker assessment than MRI and are widely available in emergencies.
Ultrasound: While less commonly used, ultrasound can help identify fluid collections and gas in the soft tissues. It is a valuable tool for guiding drainage procedures if needed.
Laboratory Tests
Laboratory tests are essential for evaluating the severity of the infection and guiding treatment. Key tests include:
Blood Tests: Complete blood count (CBC) can reveal elevated white blood cell counts, indicating infection. Other important blood tests include C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR), which are markers of inflammation.
Blood Cultures: These tests can identify the specific bacteria causing the infection, which is crucial for selecting the appropriate antibiotic therapy.
Lactate Levels: Elevated lactate levels in the blood can indicate tissue hypoxia and necrosis, common in severe infections like Fournier's gangrene.
Urine Tests: These can help assess the patient's overall health and detect any underlying urinary tract infections that might contribute to the condition.
Biopsy and Tissue Culture
In some cases, a biopsy of the affected tissue may be performed. This involves taking a small sample of the necrotic tissue for histopathological examination and culture. Tissue cultures can identify the specific pathogens involved, aiding in selecting targeted antibiotic treatments.
Diagnosing Fournier's gangrene requires a multidisciplinary approach and rapid assessment to ensure timely and effective treatment. Early diagnosis significantly improves the chances of successful management and recovery, highlighting the importance of recognizing the signs and utilizing appropriate diagnostic tools.
Fournier's Gangrene Treatment Guidelines
Treating Fournier's gangrene requires urgent and aggressive medical intervention due to its rapid progression and high mortality rate. The treatment strategy typically involves a combination of immediate medical interventions, antibiotic therapy, surgical debridement, hyperbaric oxygen therapy, and comprehensive long-term care and follow-up.
Immediate Medical Interventions
Prompt recognition and immediate treatment are crucial to improving the prognosis of Fournier's gangrene. The initial steps include:
Stabilization: Stabilize the patient by addressing any life-threatening conditions. This often involves fluid resuscitation to manage shock, electrolyte correction, and support for vital functions.
Broad-Spectrum Antibiotics: Administer broad-spectrum antibiotics when Fournier's gangrene is suspected. Early antibiotic therapy can help control the spread of infection until specific pathogens are identified through cultures.
Antibiotic Therapy
Effective antibiotic therapy is a cornerstone in the management of Fournier's gangrene. The choice of antibiotics should cover a wide range of aerobic and anaerobic bacteria commonly involved in this infection. Commonly used antibiotics include:
Broad-Spectrum Antibiotics: Initial treatment often involves a combination of antibiotics, such as piperacillin-tazobactam, metronidazole, vancomycin, or clindamycin. This combination targets Gram-positive, Gram-negative, and anaerobic bacteria.
Tailored Therapy: Once culture results are available, antibiotic therapy should be adjusted based on the specific pathogens identified and their antibiotic sensitivity profiles.
Surgical Debridement
Surgical intervention is essential and often life-saving in the treatment of Fournier's gangrene. The primary goals of surgery are to remove all necrotic tissue and reduce bacterial load. Surgical steps include:
Emergency Debridement: Immediate and aggressive debridement of all necrotic and infected tissues is critical. Multiple surgeries may be required to ensure complete removal of dead tissue.
Wound Management: Post-debridement, the wounds are often left open and managed with negative pressure wound therapy (VAC therapy) to promote healing and prevent further infection.
Reconstructive Surgery: Once the infection is controlled and the patient is stable, reconstructive surgery, including skin grafts or flaps, may be necessary to restore function and appearance.
Hyperbaric Oxygen Therapy
Hyperbaric oxygen therapy (HBOT) can be a valuable adjunct in the treatment of Fournier's gangrene. HBOT involves breathing 100% oxygen in a pressurized chamber, which increases oxygen delivery to the affected tissues. Benefits of HBOT include:
Enhanced Wound Healing: Improved oxygenation of tissues can enhance wound healing and support the body's ability to fight infection.
Reduction of Inflammation: HBOT helps reduce inflammation and edema in the affected area.
Antibacterial Effects: High oxygen levels can inhibit anaerobic bacteria's growth and enhance certain antibiotics' effectiveness.
Long-Term Care and Follow-Up
Long-term care and follow-up are essential components of managing patients recovering from Fournier's gangrene. These steps include:
Wound Care: Ongoing wound care is crucial, often involving regular dressing changes, monitoring for signs of infection, and use of wound-healing adjuncts as needed.
Rehabilitation: Physical therapy may be required to help patients regain strength and mobility, mainly if extensive tissue loss or reconstructive surgery is involved.
Monitoring and Management: Regular follow-up appointments to monitor the patient’s recovery, manage any complications, and adjust treatment plans as necessary.
Addressing Underlying Conditions: Effective management of underlying conditions, such as diabetes, a significant risk factor for Fournier's gangrene, to prevent recurrence is essential. This includes blood sugar control, lifestyle modifications, and regular medical check-ups.
Psychological Support: Providing psychological support to help patients cope with the trauma and possible disfigurement caused by Fournier's gangrene.
By following these comprehensive treatment guidelines, healthcare providers can significantly improve outcomes for patients with Fournier's gangrene. Early and aggressive intervention, coupled with meticulous long-term care, is essential in managing this severe and potentially life-threatening condition.
Prognosis and Complications
Understanding the prognosis and potential complications of Fournier's gangrene is crucial for both patients and healthcare providers. This condition, a severe and rapidly progressing necrotizing fasciitis of the perineum, requires swift medical intervention to improve outcomes and minimize the risk of life-threatening complications.
Factors Affecting Prognosis
Several factors influence the prognosis of Fournier's gangrene:
Time to Treatment: The most critical factor is the speed at which treatment is initiated. Early diagnosis and prompt surgical debridement significantly improve survival rates and reduce the extent of tissue damage.
Underlying Health Conditions: Patients with comorbidities such as diabetes, immunosuppression, chronic kidney disease, or malignancies generally have a poorer prognosis due to their compromised ability to fight infections and heal wounds.
Extent of Infection: The severity and extent of tissue involvement at diagnosis play a significant role. Extensive necrosis and deep tissue involvement are associated with higher mortality rates.
Age: Older patients tend to have a worse prognosis, likely due to decreased physiological resilience and the presence of other age-related health issues.
Nutritional Status: Malnutrition can impair immune function and wound healing, leading to worse outcomes.
Overall Health and Immune Status: A patient's general health and immune system competence are also crucial. Those with robust immune systems and better overall health are more likely to recover successfully.
Potential Complications if Untreated
If Fournier's gangrene is not promptly and adequately treated, it can lead to several severe and potentially fatal complications:
Sepsis: The infection can spread to the bloodstream, leading to sepsis, a life-threatening systemic response to infection. Sepsis can cause multi-organ failure and requires intensive care.
Systemic Inflammatory Response Syndrome (SIRS): This condition is characterized by widespread inflammation and can lead to organ dysfunction and failure if not managed aggressively.
Acute Renal Failure: The toxins produced by the infection can cause acute kidney injury, which may necessitate dialysis.
Gangrene of Surrounding Tissues: The infection can spread to adjacent tissues, leading to further necrosis and the need for more extensive surgical debridement.
Death: Without timely and appropriate treatment, Fournier's gangrene can be fatal. Mortality rates can be as high as 20-40%, depending on the severity and speed of intervention.
Recovery Outcomes
The recovery outcomes for patients with Fournier's gangrene vary widely based on several factors, including the severity of the initial infection, the timeliness of treatment, and the patient's overall health. Key points regarding recovery include:
Survival Rates: With prompt and aggressive treatment, many patients can survive Fournier's gangrene. Survival rates improve significantly with early diagnosis and immediate surgical intervention.
Functional Recovery: Post-recovery, patients may experience varying degrees of functional impairment depending on the extent of tissue removal and the areas affected. Rehabilitation and physical therapy can aid in regaining function and mobility.
Wound Healing: The healing of surgical wounds can be prolonged, especially in patients with diabetes or other conditions that affect wound healing. Regular follow-up care and wound management are essential to prevent secondary infections and promote healing.
Psychological Impact: The psychological impact of the disease and its treatment, which may include extensive tissue loss and disfigurement, can be significant. Counseling and support groups may be beneficial for emotional and mental health recovery.
Quality of Life: Long-term quality of life can be affected, particularly if significant reconstructive surgery is required. Ongoing medical care and lifestyle adjustments may be necessary to manage lasting effects.
Importance of Managing Underlying Conditions
Diabetes Management: Diabetes is a significant risk factor for Fournier's gangrene. Proper blood glucose management through medication, diet, and regular monitoring can reduce the risk of infections. Patients should also have regular foot and skin exams to identify potential issues early.
Immune System Health: Conditions that weaken the immune system, such as HIV/AIDS or the use of immunosuppressive medications, can increase the risk of severe infections. Managing these conditions under the guidance of a healthcare provider is crucial.
Chronic Illness Management: Conditions like chronic kidney disease, liver disease, and obesity can also increase the risk. Proper management of these conditions through medication, lifestyle changes, and regular medical supervision can help mitigate the risk.
Lifestyle Changes to Reduce Risk
Healthy Diet and Exercise: A balanced diet and regular exercise can help maintain overall health, strengthen the immune system, and manage underlying conditions like diabetes and obesity. These factors collectively reduce the risk of infections.
Quitting Smoking: Smoking impairs blood circulation and immune function, increasing the risk of infections. Quitting smoking can improve overall health and reduce the risk of severe infections like Fournier's gangrene.
Limiting Alcohol Intake: Excessive alcohol consumption can weaken the immune system and increase the risk of infections. Moderation in alcohol consumption can help maintain a healthy immune response.
Stress Management: Chronic stress can weaken the immune system. Stress management techniques such as mindfulness, meditation, and regular exercise can help maintain a healthy immune system and reduce infection risk.
Adhering to these prevention strategies can significantly lower individuals' risk of developing Fournier's gangrene. Managing underlying health conditions, maintaining good personal hygiene, and adopting healthy lifestyle changes are crucial steps in preventing this life-threatening condition. Regular medical consultations and prompt treatment of infections can further enhance prevention efforts, ensuring better overall health and well-being.
Conclusion
Fournier's gangrene is a severe and potentially life-threatening condition that necessitates immediate medical attention. Understanding the causes, risk factors, and symptoms of Fournier's gangrene is crucial for early detection and effective treatment. Prompt diagnosis and aggressive medical and surgical interventions can significantly improve patient outcomes. It's essential to manage underlying conditions like diabetes and maintain good hygiene to prevent the onset of this infection. If any symptoms of Fournier's gangrene are present, seeking urgent medical help is imperative to mitigate complications and ensure a better prognosis.


.webp)

.avif)