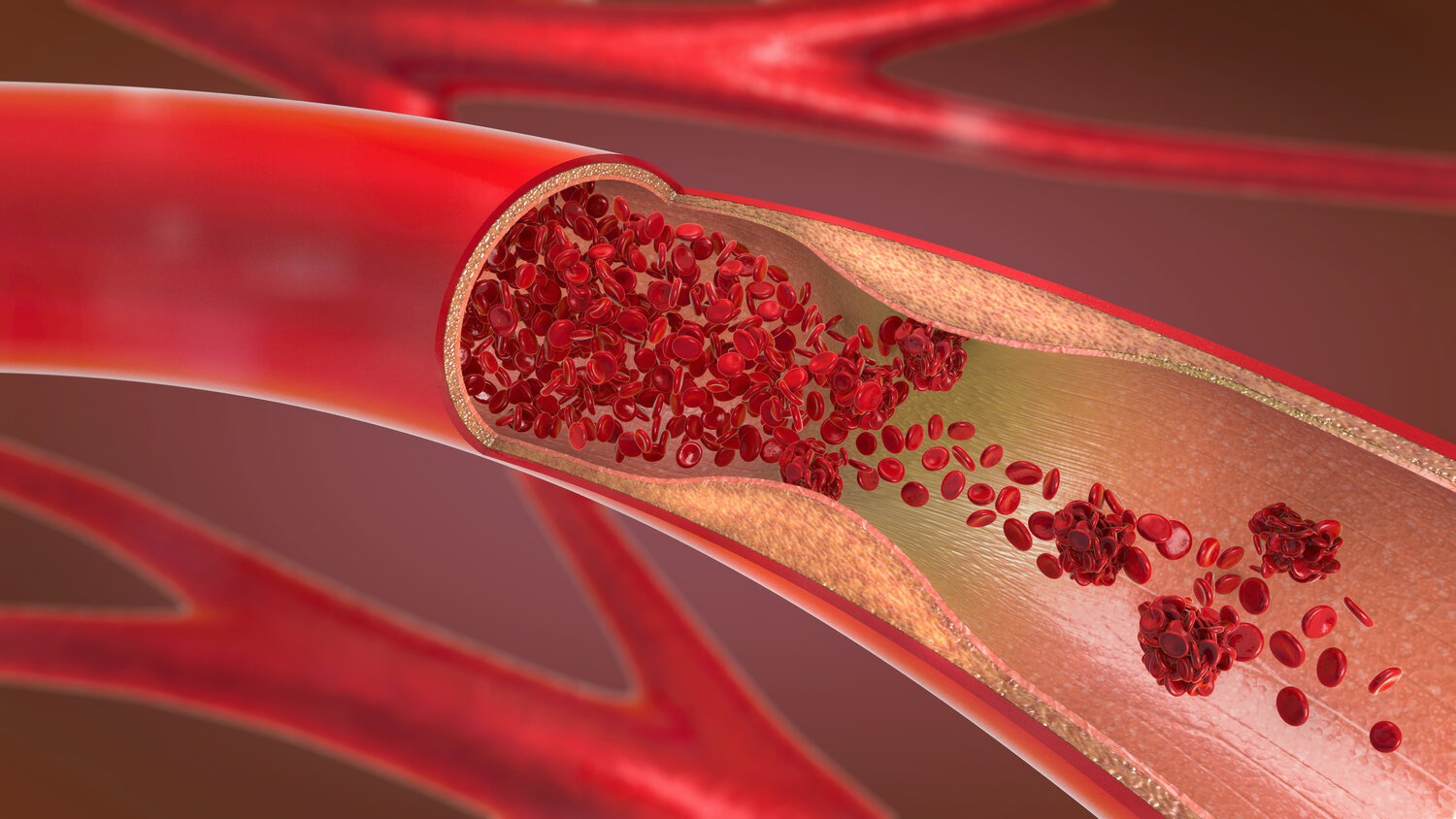
Peripheral Vascular Disease (PVD) refers to disorders affecting the blood vessels outside the heart and brain, particularly the arteries, veins, and lymphatic vessels in the extremities. The most common type of PVD is caused by atherosclerosis, where fatty deposits build up on the walls of arteries, narrowing them and reducing blood flow. This condition primarily affects the legs and feet, leading to symptoms such as pain, numbness, and, in severe cases, tissue damage or gangrene. Understanding peripheral vascular disease is essential because it can significantly impact a person’s quality of life and, if left untreated, can lead to severe complications, including limb loss and increased risk of heart attack or stroke.
Prevalence and Risk Factors
Peripheral Vascular Disease is a widespread condition, particularly among older adults. It is estimated that millions of people worldwide are affected by PVD, with the prevalence increasing with age. Key risk factors include smoking, which is the most significant modifiable risk factor, as it contributes to the development and progression of atherosclerosis. Diabetes is another significant risk factor, as high blood sugar levels can damage blood vessels, making individuals more susceptible to PVD. Other contributing factors include high blood pressure, high cholesterol, obesity, and a sedentary lifestyle. Family history and genetic predisposition can also play a role in increasing the risk of developing PVD. Understanding these risk factors is crucial for early detection, prevention, and effective management of the condition.
Types of Peripheral Vascular Disease
Atherosclerotic PVD
Atherosclerotic Peripheral Vascular Disease (PVD) is the most prevalent form of PVD, primarily caused by atherosclerosis—a condition in which fatty deposits, known as plaques, accumulate on the inner walls of the arteries. This buildup narrows the arteries, restricting blood flow to the limbs, particularly the legs. Over time, this can lead to critical reductions in oxygen and nutrient supply to the tissues, which may cause claudication, characterized by pain, cramping, or leg fatigue during physical activity. As the disease progresses, symptoms may worsen, with pain occurring even at rest and more severe complications such as non-healing ulcers, infections, and in extreme cases, gangrene, which may necessitate amputation. Atherosclerotic PVD is closely linked to cardiovascular diseases like coronary artery disease, and those with PVD are at an elevated risk for heart attacks and strokes.
Non-Atherosclerotic PVD
Non-Atherosclerotic Peripheral Vascular Disease encompasses various conditions that affect the peripheral blood vessels but are not caused by atherosclerosis. Two notable forms of non-atherosclerotic PVD are Buerger's disease and Raynaud’s phenomenon.
Buerger's disease, also known as thromboangiitis obliterans, is a rare inflammatory condition that affects small and medium-sized arteries and veins in the limbs. It is strongly associated with tobacco use, and its hallmark symptoms include pain, especially in the hands and feet, due to reduced blood flow. As the disease advances, it can lead to ulcerations and gangrene, often necessitating amputation if smoking is not ceased.
On the other hand, Raynaud's phenomenon is a condition where small blood vessels in the fingers and toes constrict excessively in response to cold or stress. This leads to episodes of reduced blood flow, causing the affected areas to turn white or blue and become cold and numb. While Raynaud’s is generally less severe than other forms of PVD, chronic cases can lead to sores or ulcers if blood flow is repeatedly compromised.
Key Differences from Atherosclerotic PVD
The critical differences between atherosclerotic and non-atherosclerotic PVD are their causes, affected vessels, and progression. Atherosclerotic PVD is directly linked to the buildup of plaques in larger arteries, leading to chronic and progressive narrowing that affects blood flow. In contrast, non-atherosclerotic forms like Buerger's disease and Raynaud’s phenomenon typically involve smaller vessels and result from inflammatory or spastic processes rather than plaque accumulation. The symptoms and complications also differ, with atherosclerotic PVD often leading to more severe outcomes, such as limb ischemia. At the same time, non-atherosclerotic PVD may primarily cause discomfort or episodic symptoms with a less direct threat to limb viability, except in severe or unmanaged cases. Understanding these differences is crucial for accurate diagnosis and appropriate treatment of peripheral vascular disease.
Peripheral Vascular Disease Symptoms
Early Symptoms
Peripheral Vascular Disease (PVD) often begins with subtle symptoms that can easily be overlooked or mistaken for other conditions. One of the earliest and most common symptoms is claudication, characterized by pain, cramping, or a sense of fatigue in the muscles of the legs or arms during physical activity, such as walking or climbing stairs. This pain typically subsides with rest and recurs with exertion, as it is caused by inadequate blood flow to the muscles due to narrowed arteries. In addition to claudication, individuals with early-stage PVD may experience numbness, tingling, or a sensation of coldness in the extremities, particularly the feet and toes. These symptoms result from reduced oxygen and nutrient supply to the tissues and can indicate the presence of atherosclerosis or other forms of vascular impairment.
Advanced Symptoms
As peripheral vascular disease progresses, the symptoms become more severe and can lead to significant complications. One of the hallmark signs of advanced PVD is the development of non-healing wounds or sores on the legs and feet. These wounds, often called ulcers, occur because the reduced blood flow impairs the body’s ability to heal even minor injuries. If left untreated, these wounds can become infected and may lead to gangrene, a severe condition where tissue dies due to lack of blood supply. Critical limb ischemia (CLI) is the most severe form of PVD, characterized by persistent pain at rest, extensive ulceration, and gangrene. CLI is a medical emergency that requires immediate intervention to restore blood flow and prevent limb loss. The progression from early symptoms like claudication to advanced conditions such as gangrene underscores the importance of early detection and treatment of PVD.
Impact on Quality of Life
The symptoms of peripheral vascular disease can profoundly impact an individual’s quality of life. Early-stage symptoms like claudication may limit physical activity, causing individuals to reduce or avoid exercise due to discomfort, leading to a sedentary lifestyle and exacerbating the condition. As the disease progresses, the pain and discomfort associated with non-healing wounds and critical limb ischemia can severely restrict mobility, making daily activities such as walking, standing, or even sleeping difficult. The constant pain and risk of complications also contribute to a decline in overall well-being, leading to increased anxiety, depression, and social isolation. The potential for limb loss in advanced PVD adds to the psychological and emotional burden, highlighting the need for comprehensive management strategies to improve both physical and mental health outcomes for those affected by peripheral vascular disease.
Diagnosis of Peripheral Vascular Disease
Clinical Evaluation
Peripheral Vascular Disease (PVD) diagnosis begins with a comprehensive clinical evaluation. This involves taking a detailed patient history and conducting a thorough physical examination to identify risk factors and symptoms indicative of PVD.
Patient History: The clinician will inquire about the patient's medical history, including any existing conditions such as diabetes, hypertension, hyperlipidemia, or smoking habits, which are significant risk factors for PVD. The patient may report symptoms such as intermittent claudication, muscle pain, or leg cramping during physical activity, which typically subsides with rest. Additionally, the clinician will explore these symptoms' duration, frequency, severity, and associated signs like numbness, coldness, or non-healing wounds on the lower extremities.
Physical Examination: A thorough physical examination focuses on the cardiovascular and peripheral vascular systems. The clinician will palpate pulses in the legs, feet, and arms, assessing their strength and symmetry. A diminished or absent pulse in the lower extremities may suggest arterial blockages. Additionally, the examination may reveal signs such as skin discoloration, atrophy, ulcers, or temperature differences between the limbs, which can indicate impaired blood flow.
Diagnostic Tests
After the initial clinical evaluation, specific diagnostic tests are employed to confirm the presence and severity of Peripheral Vascular Disease. These tests help to assess blood flow and identify blockages or narrowing of the arteries.
Ankle-Brachial Index (ABI): The ABI is a simple, non-invasive test that compares the blood pressure in the ankle with the blood pressure in the arm. It is a critical tool for diagnosing PVD. A blood pressure cuff is placed on both the arm and the ankle, and measurements are taken using a Doppler device. The ABI is calculated by dividing the systolic blood pressure at the ankle by the systolic blood pressure at the arm. An ABI of less than 0.90 typically indicates the presence of PVD, with lower values suggesting a more severe disease.
Doppler Ultrasound: This test uses high-frequency sound waves to create images of the blood vessels and measure blood flow through them. A Doppler ultrasound can detect areas of reduced or blocked blood flow in the arteries, essential for assessing the severity of PVD. The test is non-invasive, painless, and provides valuable information about the blood flow velocity and arterial obstructions.
Angiography: In cases where more detailed imaging is required, angiography is performed. This test involves injecting a contrast dye into the bloodstream, followed by X-ray imaging. Angiography provides a clear and detailed view of the blood vessels, allowing clinicians to identify the exact location and extent of arterial blockages or narrowing. It is particularly useful when planning interventions such as angioplasty or bypass surgery.
Treatment Options for Peripheral Vascular Disease
Peripheral Vascular Disease (PVD) management is multifaceted, focusing on alleviating symptoms, improving quality of life, and preventing disease progression. Treatment options include lifestyle modifications, medications, and surgical interventions tailored to the severity of the condition and the patient's needs.
Lifestyle Modifications
Lifestyle changes form the cornerstone of PVD treatment, particularly for patients with mild to moderate disease. These modifications aim to reduce risk factors, improve circulation, and slow the progression of arterial blockages.
Smoking Cessation: Smoking is one of the most significant risk factors for PVD, as it contributes to the development and progression of atherosclerosis, the underlying cause of the disease. Quitting smoking is essential for slowing the advancement of PVD and reducing the risk of complications such as heart attacks or strokes. Patients should be encouraged to seek support through smoking cessation programs, medications, or counseling to quit smoking successfully.
Exercise: Regular physical activity, particularly a supervised exercise program, is highly beneficial for patients with PVD. Exercise, such as walking, helps improve circulation by promoting the development of collateral blood vessels, which can bypass blockages. Patients are often advised to engage in structured walking programs until moderate pain develops, rest until it subsides, and resume walking. Over time, this can increase walking distance and reduce symptoms of intermittent claudication.
Dietary Changes: Adopting a heart-healthy diet is another critical aspect of managing PVD. A diet low in saturated fats, trans fats, and cholesterol can help control blood lipid levels while reducing salt intake, aiding blood pressure management. Incorporating plenty of fruits, vegetables, whole grains, and lean proteins into the diet supports overall cardiovascular health and helps mitigate the effects of PVD. Patients may also be advised to manage their weight, as obesity is a contributing factor to the disease.
Medications
Medications play a vital role in managing Peripheral Vascular Disease, particularly in controlling symptoms, preventing clot formation, and managing associated risk factors.
Antiplatelet Agents: These medications, such as aspirin or clopidogrel, help prevent the formation of blood clots in narrowed arteries, reducing the risk of heart attacks and strokes in PVD patients. By inhibiting platelet aggregation, these drugs help maintain blood flow through partially blocked vessels and reduce the likelihood of acute arterial occlusion.
Statins: Statins are cholesterol-lowering medications that are commonly prescribed to patients with PVD. They work by reducing the levels of low-density lipoprotein (LDL) cholesterol in the blood, which slows the progression of atherosclerosis. Additionally, statins have anti-inflammatory properties that can stabilize plaques within the arteries, reducing the risk of rupture and subsequent complications.
Blood Pressure Control: Managing hypertension is crucial for patients with PVD, as high blood pressure can exacerbate arterial damage and worsen the disease. Medications such as ACE inhibitors, angiotensin II receptor blockers (ARBs), beta-blockers, or calcium channel blockers may be prescribed for optimal blood pressure control. Keeping blood pressure within target ranges helps prevent further damage to blood vessels and reduces the overall cardiovascular risk.
Surgical Interventions
In cases where PVD is severe or unresponsive to conservative treatment, surgical interventions may be necessary to restore adequate blood flow and prevent limb-threatening complications.
Bypass Surgeries: Surgical bypass is a procedure in which a graft from another part of the patient's body or a synthetic material creates a new pathway for blood to flow around a blocked artery. This procedure is particularly effective for long or complex blockages that cannot be treated with less invasive methods. During the surgery, the blocked segment of the artery is bypassed, and blood is rerouted through the graft to restore circulation to the affected limb.
Endarterectomy: Endarterectomy is a surgical procedure in which the inner lining of an artery and the plaque causing the blockage is removed. This procedure is often used when blockage is localized and accessible. The removal of the plaque restores normal blood flow through the artery and alleviates symptoms of PVD. Endarterectomy is commonly performed on carotid arteries but can also be applied to peripheral arteries.
Angioplasty and Stenting: Angioplasty is a minimally invasive procedure involving a balloon catheter to dilate a narrowed or blocked artery. The balloon is inflated at the site of the blockage, compressing the plaque against the artery walls and widening the vessel. In many cases, a stent, a small metal mesh tube, is placed in the artery to keep it open after angioplasty. This procedure is particularly effective for treating localized blockages and can significantly improve blood flow and symptom relief.
Other Vascular Procedures: Additional procedures like atherectomy may remove plaque from the arteries using a rotating cutting device or laser. These procedures are often combined with angioplasty and stenting to achieve optimal results. More complex surgical interventions may be required in more advanced cases, where limb salvage is the primary goal.
Preventing Peripheral Vascular Disease
Peripheral vascular disease (PVD) can significantly impact a person's quality of life and lead to severe complications if left untreated. Fortunately, PVD is largely preventable through lifestyle modifications and effective management of risk factors. By adopting preventive measures and emphasizing early detection, individuals can reduce their risk of developing PVD and its associated complications.
Preventive Measures
Prevention of Peripheral Vascular Disease involves a proactive approach to health, focusing on lifestyle changes and managing underlying risk factors that contribute to the development of the disease.
Regular Exercise and Physical Activity: Regular physical activity is one of the most effective ways to prevent PVD. Exercise improves circulation, promotes cardiovascular health, and helps maintain a healthy weight, crucial in reducing the risk of PVD. Walking, jogging, cycling, and swimming are particularly beneficial as they enhance blood flow to the lower extremities, which PVD often compromises. Aim for at least 30 minutes of moderate-intensity exercise most days of the week to achieve these benefits.
Healthy Diet and Weight Management: A balanced diet prevents PVD. A diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats can help manage cholesterol levels, blood pressure, and blood sugar—critical factors in preventing atherosclerosis, the underlying cause of PVD. Limiting intake of saturated fats, trans fats, and added sugars can further reduce the risk of plaque buildup in the arteries. Maintaining a healthy weight through proper diet and exercise is also crucial, as obesity is a significant risk factor for PVD and other cardiovascular diseases.
Managing Risk Factors: Effective management of risk factors is critical in preventing Peripheral Vascular Disease. This includes:
Hypertension: High blood pressure is a significant contributor to the development of PVD, as it can damage the blood vessel walls and accelerate the process of atherosclerosis. Regular monitoring and management of blood pressure through lifestyle changes and medications, if necessary, can help prevent PVD.
Diabetes: Individuals with diabetes are at a higher risk of developing PVD due to the damaging effects of high blood sugar on the blood vessels. Tight control of blood sugar levels through diet, exercise, and medication is essential in reducing the risk of PVD in diabetic patients.
Smoking Cessation: Smoking is a significant modifiable risk factor for PVD. The chemicals in tobacco smoke damage blood vessels and promote the formation of plaques, leading to arterial narrowing. Quitting smoking is one of the most effective ways to prevent PVD and improve overall cardiovascular health.
Cholesterol Management: High levels of low-density lipoprotein (LDL) cholesterol contribute to the formation of atherosclerotic plaques. Managing cholesterol levels through diet, exercise, and, if necessary, medications like statins can help prevent PVD.
Importance of Early Detection
Early detection of Peripheral Vascular Disease is crucial for preventing its progression and associated complications. Timely diagnosis allows for early intervention, which can significantly improve patient outcomes.
Screening Recommendations for At-Risk Individuals: PVD screening is recommended for individuals at higher risk of developing the disease. This includes those with a history of smoking, diabetes, hypertension, high cholesterol, or a family history of cardiovascular disease. Screening may also be advised for individuals over 50, particularly if they have other risk factors. Common screening methods include the Ankle-Brachial Index (ABI), which compares blood pressure in the ankle and arm to detect blockages, and Doppler ultrasound, which assesses blood flow in the arteries.
Benefits of Early Intervention in PVD: Early intervention in PVD can prevent the progression of the disease and reduce the risk of serious complications such as critical limb ischemia, gangrene, or the need for amputation. By identifying PVD in its early stages, healthcare providers can implement lifestyle modifications, medications, or minimally invasive procedures to restore blood flow and improve symptoms. Early treatment can also help prevent cardiovascular events such as heart attacks and strokes, which are commonly associated with PVD.
Living with Peripheral Vascular Disease
Living with Peripheral Vascular Disease (PVD) requires a comprehensive approach to managing symptoms, monitoring disease progression, and taking proactive steps to prevent complications. With the right strategies, individuals can maintain a good quality of life despite the challenges posed by PVD.
Managing Symptoms
Effective management of the symptoms associated with Peripheral Vascular Disease is crucial for improving daily functioning and reducing discomfort. Symptoms like pain, cramping, and non-healing wounds are common, and addressing them promptly can help prevent more severe complications.
Pain Management: One of the primary symptoms of PVD is intermittent claudication—pain or cramping in the legs during physical activity, which typically eases with rest. Pain management strategies may include:
Medications: Pain relievers and medications that improve blood flow, such as cilostazol, may be prescribed to help alleviate claudication symptoms. These medications widen blood vessels and reduce viscosity, making blood flow through narrowed arteries easier.
Exercise Therapy: Structured exercise programs, particularly supervised walking, reduce pain and improve mobility. These programs involve walking until moderate pain develops, resting, and then resuming walking. Over time, this approach can increase walking distance and reduce the severity of symptoms.
Lifestyle Modifications: Quitting smoking and managing risk factors like diabetes and hypertension can also help reduce pain and slow the progression of PVD.
Physical Therapy: Physical therapy plays a significant role in managing PVD symptoms. A physical therapist can design a customized exercise plan that includes stretching, strength training, and aerobic exercises to improve circulation, increase stamina, and reduce the risk of complications. Additionally, physical therapy can help improve overall mobility and reduce the likelihood of falls or injuries related to muscle weakness.
Wound Care: Individuals with PVD are at a higher risk of developing non-healing wounds or ulcers, particularly on the lower extremities. Proper wound care is essential to prevent infections and promote healing. This may involve:
Regular Cleaning and Dressing: Keeping wounds clean and adequately dressed is vital to prevent infection. Specialized dressings that maintain a moist environment can promote faster healing.
Monitoring for Infection: It is crucial to watch for signs of infection, such as increased redness, swelling, warmth, or pus. To prevent further complications, infections should be treated promptly with appropriate antibiotics.
Consulting Wound Care Specialists: Consulting with a wound care specialist may be necessary for chronic or severe wounds. These professionals can provide advanced treatments, such as debridement (removal of dead tissue) or hyperbaric oxygen therapy, to aid in healing.
Monitoring Disease Progression
Regular monitoring of Peripheral Vascular Disease is essential to detect any worsening of the condition and adjust treatment plans accordingly. By staying vigilant and attending regular follow-ups, patients can manage PVD more effectively and prevent serious complications.
Importance of Regular Follow-Ups: Regular follow-up appointments with healthcare providers are critical for managing PVD. During these visits, clinicians will assess the effectiveness of current treatments, monitor for any new or worsening symptoms, and adjust medications or therapies as needed. Follow-ups may include:
Physical Exams: Checking pulses, skin condition, and any new symptoms that may indicate changes in blood flow.
Imaging Tests: Doppler ultrasound or ankle-brachial index (ABI) measurements may be repeated to evaluate blood flow and detect disease progression.
Medication Review: Evaluating the effectiveness of current medications and making adjustments to ensure optimal blood pressure, cholesterol levels, and blood glucose control.
Recognizing Signs of Worsening Disease: Individuals with PVD need to be aware of the signs that may indicate worsening of the disease. Early recognition of these signs can prompt timely intervention and prevent complications. Signs to watch for include:
Increased Pain: Worsening pain, particularly at rest or during the night, may indicate a progression of PVD to a more severe form, such as critical limb ischemia.
Non-Healing Wounds or Ulcers: The appearance of new wounds or ulcers that do not heal within a few weeks should be addressed immediately, as they may signal a significant reduction in blood flow.
Color or Temperature Changes: Changes in the color (paleness, bluish tint) or temperature (coolness) of the affected limb can indicate reduced blood flow and should be reported to a healthcare provider.
Numbness or Tingling: New or worsening numbness, tingling, or a feeling of heaviness in the legs can be signs of deteriorating circulation and should not be ignored.
Conclusion
Peripheral Vascular Disease (PVD) is a severe condition characterized by the narrowing of blood vessels, primarily in the legs, which can lead to symptoms such as pain, cramping, and non-healing wounds. Effective management of PVD involves a combination of lifestyle modifications, medications, and surgical interventions to restore blood flow and prevent complications. Early diagnosis and treatment are critical in slowing the progression of the disease and improving patient outcomes. Recognizing symptoms early and seeking timely medical advice can make a significant difference in managing PVD. It is essential for individuals at risk or experiencing symptoms to consult healthcare professionals for a tailored care plan that addresses their specific needs, ensuring the best possible quality of life.


.webp)

.avif)