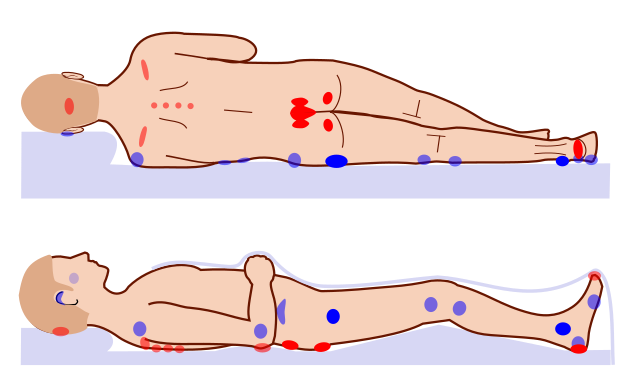
Pressure injuries, also known as pressure ulcers or bedsores, are a significant health problem that affects an estimated 3 million adults in the United States alone. They are costly and challenging for both patients and healthcare professionals to manage. Pressure injuries occur when the skin and underlying tissues are subject to prolonged pressure, typically in areas of the body that are prone to high levels of friction or shear. They are seen in people who are bedridden or have limited mobility but can also occur in people who can move around but do not receive proper care.
Pressure injuries can range in severity from mild skin redness to deep wounds that reach the muscle and bone.
Prevention of pressure injuries is crucial, as they can be challenging to heal and are prone to complications such as infection and sepsis. Proper wound care management is important to prevent them and to promote the healing of existing wounds. It is also essential to involve healthcare professionals and follow their recommendations for wound care. Following these guidelines can help prevent pressure injuries and improve the quality of life for those at risk.
In this blog post, we'll discuss what pressure injuries are in more detail, their varying stages, the importance of prevention, and how to prevent them.
Let's get started.
What Are Pressure Injuries?
Pressure injuries are sores, also known as ulcers. They are skin tissue injuries that occur on areas of your skin that form because of prolonged pressure over specific areas of your body.
They are commonly termed bedsores and are experienced by people with decreased mobility, making posture changes challenging.
Bedsores or pressure injuries are primarily caused by loss of sensory perception, decreased mobility, and prolonged loss of consciousness. This is because patients are unaware of their discomfort and cannot relieve the pressure. But this is not limited to adults, this may also occur with infants and children who are at a higher risk because of their relatively larger surface skin area and their increased nutritional requirements as well as possible nutritional deficiencies.
There are two factors to pressure injuries, both internal and external factorials. External factors include; friction, pressure, moisture, and force. In contrast, internal factors may include malnutrition, anemia, fever, and endothelial dysfunction, which can speed up the process of these injuries.
A bedridden patient or a patient undergoing surgery for as little as two hours is already susceptible.
The regulatory mechanism of the nervous system is responsible for regulating the local blood flow, and it plays a role in forming these lesions. Prolonged pressure on your skin or tissues may cause capillary bed occlusions, lowering oxygen levels in that area. The ischemic tissue will then accumulate toxic metabolites, which is the foundation for tissue ulcers and necrosis.
Patients with the following conditions are prone to pressure ulcers:
- Neurologic disease
- Malnutrition
- Cardiovascular disease
- Dehydration
- Prolonged anesthesia
- Hypotension
- Surgical patients
What Are The 4 Stages Of Pressure Injuries?
There are various stages of pressure injury, and they are classified based on the depth of the skin injury.
The 4 stages of pressure injuries are:
Stage 1: The skin is red and warm to the touch. It may be itchy with a burning sensation. .
Stage 2: The concerned skin area is more damaged with partial loss of skin thickness or a scrape, an open sore, or even a blister.
Stage 3: The area is damaged with a crater-like appearance from the skin damage involving the subcutaneous fat or below the skin's surface.
Stage 4: The concerned skin area is severely damaged by a large wound involving muscle and/or bone.
Why Is Preventing Pressure Injuries Extremely Important?
Pressure injuries are still a significant health concern affecting many people. It has one of the highest occurrence rates. Considering the aging population, nursing shortage, and our fragmented care, the incidences of pressure ulcers or bedsores will most likely remain and continue to rise.
Bedsores vary greatly depending on the healthcare setting, and the cost to treat pressure injuries can be very expensive.
The Healthcare Cost and Utilization Project, also known as the HCUP, reports that treating pressure injuries is 2.5 times more expensive than preventing them.
Besides the high cost of treating bedsores, the other effect of these lesions is infections that can significantly impact the patient's life. Several studies found mortality rates as high as 60% for elderly adults with pressure injuries within a year after hospital discharge. Often, the lesion does not cause death but may develop after a decline in the patient's health.
How To Prevent Pressure Injuries?
Many clinicians or healthcare providers believe that developing pressure injuries is not solely the responsibility of nurses but the entire healthcare setting or system.
Preventing pressure ulcers or bedsores requires an interdisciplinary approach while considering a customized plan tailored specifically to each patient.
But generally, certain practices can be followed routinely to prevent bedsores, such as;
- Repositioning and turning every 2 hours.
- Changing the position in a wheelchair every 15 minutes.
- Soft padding in beds or wheelchairs to reduce pressure.
- Good skin care can also keep the skin dry and clean.
- Good nutrition is necessary because enough vitamins, calories, protein, minerals, and fluid will make it difficult for the lesions to heal and recover, no matter how well you try and take care of them.
Summing It Up
In conclusion, pressure injuries are a common and severe problem that can have significant physical and emotional consequences for those affected. They are caused by prolonged pressure on the skin and underlying tissues and are often seen in people who are bedridden or have limited mobility. Proper wound care management is essential to prevent pressure injuries and to promote the healing of existing wounds. This includes:
- Regularly turning and repositioning the person to reduce pressure.
- Keeping the skin clean and moisturized.
- Using specialized devices and dressings as needed.
It is also important to involve healthcare professionals and follow their recommendations for wound care. Following these guidelines can help prevent pressure injuries and improve the quality of your life for those at risk.


.webp)

.avif)